PLEASE NOTE:
While the following article relates to your Google search, the services and methods at Goodwin Hypnosis may differ from those mentioned below. Since 2007, we have helped thousands of clients to overcome emotional and behavioral challenges when all else had failed. According to many of them (and their referring healthcare providers), our methods are faster than talk therapy, easier than willpower, and safer than medication. If you’re ready to resolve your issues, skip the article and visit the rest of our website, where you can learn about our unique approach, watch client testimonial videos, and discover how working with us one-on-one could be the solution you’ve been searching for.
We can help you with a variety of issues relating to emotional trauma. While we don't diagnose disorders like PTSD, we have helped hundreds of clients to overcome a wide range of traumatic experiences and their negative effects with methods that are more efficient and comfortable than CBT or EMDR. If you would like to learn more about working with us one-on-one to clear your trauma, click here.
Introduction
The struggle between PTSD and insomnia is a complex and often debilitating reality for many individuals. As the shadows of trauma loom large, they can disrupt the most fundamental aspect of well-being: sleep. The connection between these two conditions is not merely coincidental; it is a profound interplay that demands attention and understanding.
With a staggering percentage of those affected by PTSD experiencing significant sleep disturbances, the implications extend far beyond fatigue, affecting emotional regulation, cognitive function, and overall quality of life. By delving into the mechanisms behind this connection and exploring effective strategies for managing insomnia, individuals can reclaim their nights and embark on a path toward healing. This article illuminates the intricate relationship between PTSD and sleep disturbances, offering insights and support for those seeking relief and restoration.
The Intricate Link Between PTSD and Insomnia
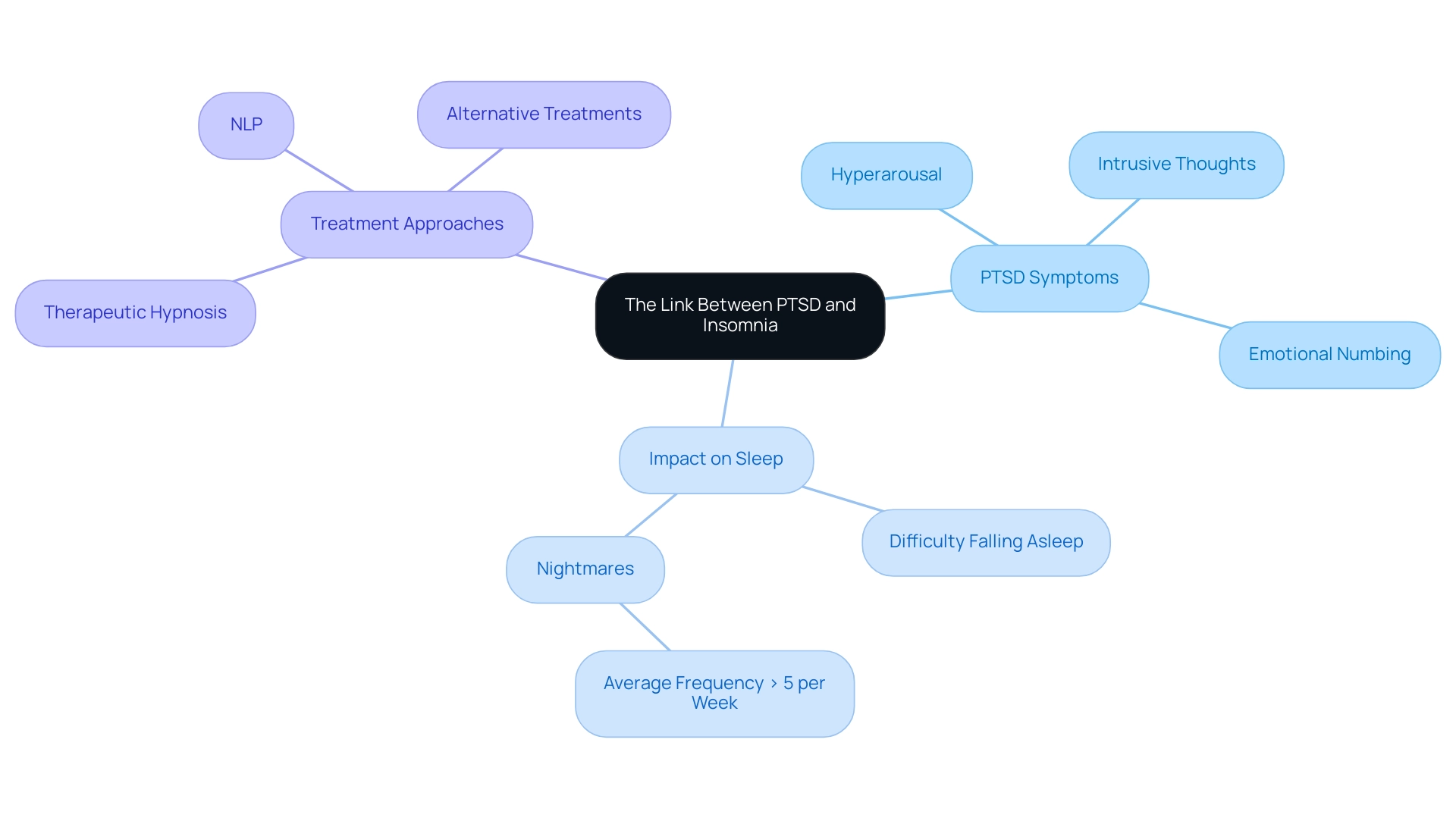
Post-traumatic stress disorder frequently presents with various symptoms, such as hyperarousal, intrusive thoughts, and emotional numbing, all of which can greatly interfere with rest patterns. Many individuals may struggle with falling asleep due to overwhelming anxiety or the haunting presence of nightmares, with studies indicating that those with trauma experience an average of more than five nightmares per week. This pattern of rest disruptions can worsen other trauma-related symptoms, making it progressively harder to achieve relief and comfort.
Dr. Erin Koffel emphasizes that "Sleep disturbances are considered a modifiable risk factor for onset and relapse of mental disorders," underscoring the critical importance of addressing these issues within the context of trauma treatment. Furthermore, recent findings suggest that sleep disturbances may hinder emotional regulation and contribute to trauma-related symptoms by affecting the consolidation of emotional memories and impairing extinction learning.
Recognizing this crucial link empowers trauma seekers to confront their insomnia not merely as a standalone issue but as a vital component of their healing journey. Engaging with this understanding can lead people like Amber, who conquered debilitating trauma and grief through innovative techniques, to seek appropriate strategies and support, ultimately aiding in their path toward recovery.
With hypnosis and NLP, many clients have transformed limiting beliefs and addressed deeply rooted emotional and behavioral issues, highlighting the potential for profound healing. Notably, anxiety disorders affect 40 million American adults, with a significant portion experiencing challenges in traditional therapies such as talk therapy or CBT, which may not adequately address their needs. This highlights the importance of exploring alternative approaches like hypnosis for those seeking effective solutions.
Effective Strategies for Managing PTSD-Related Insomnia
-
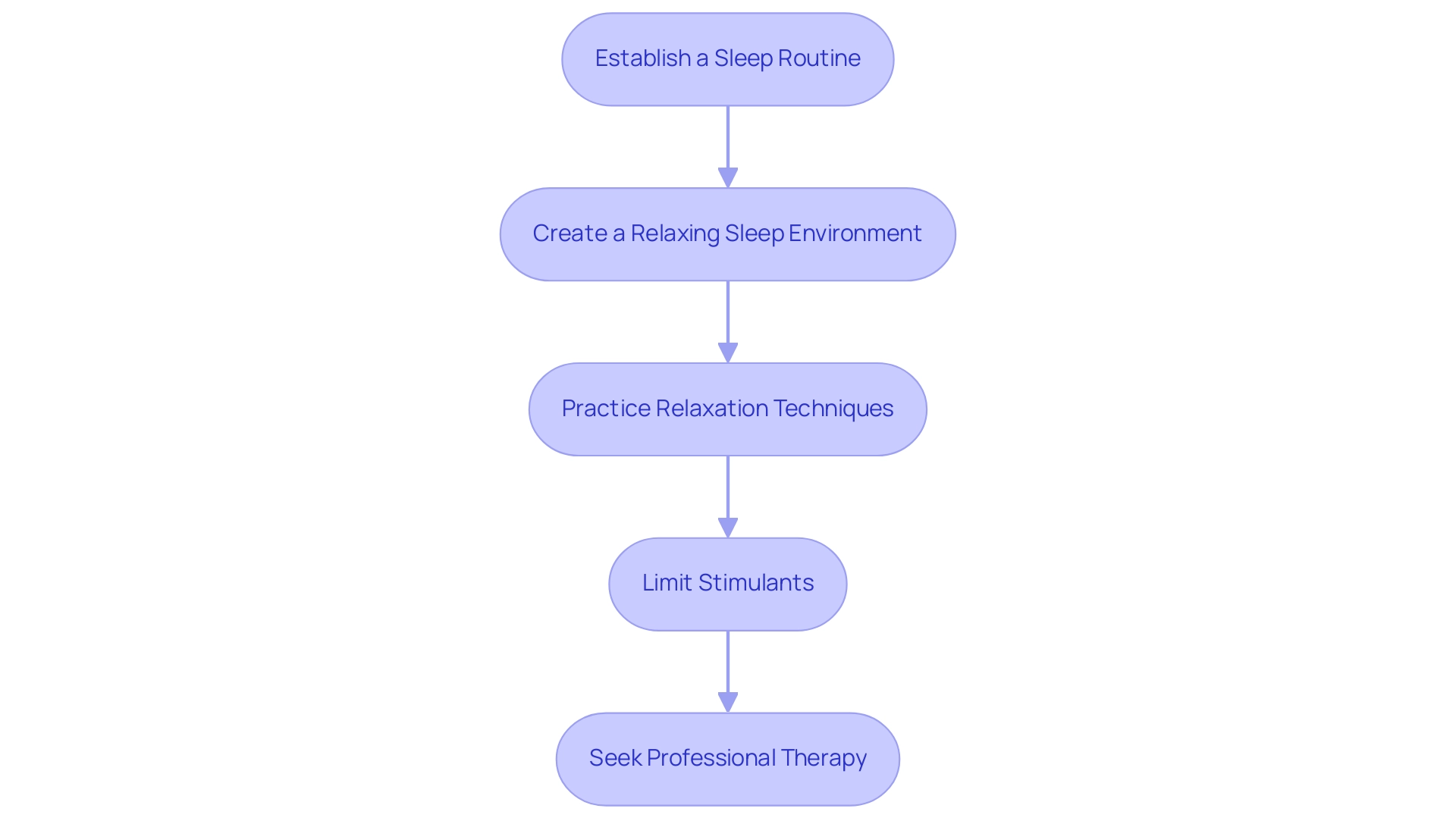
Establish a Sleep Routine: Consistency is vital for your well-being. Aim to go to bed and wake up at the same time every day, which helps regulate your body’s internal clock. This routine can significantly enhance your rest quality, making it easier to fall into slumber and wake refreshed, especially for those affected by PTSD and anxiety.
-
Create a Relaxing Sleep Environment: Transform your bedroom into a sanctuary dedicated to rest. Ensure it is dark, quiet, and cool, creating a space that invites relaxation. Consider using white noise machines or blackout curtains to eliminate distractions and promote a sense of calm, which is crucial for individuals experiencing emotional trauma.
-
Practice Relaxation Techniques: Engaging in deep breathing, meditation, or gentle yoga before bedtime can help soothe your mind and body. Research has demonstrated that such relaxation methods can enhance rest quality by up to 30%, alleviating anxiety and tension, and paving the way for a more restful night. Hypnosis, as evidenced by client testimonials, has shown transformative effects on anxiety relief and emotional healing, offering a holistic approach to relaxation. Clients have reported significant improvements in their ability to unwind and achieve restful rest after incorporating these techniques into their routines.
-
Limit Stimulants: Be mindful of your consumption of caffeine and nicotine, especially in the hours leading up to bedtime. Substantial meals or alcohol near bedtime can interfere with your rest, so try to limit these as well, allowing your body to unwind naturally. Comprehending the reasons for sleeplessness can empower individuals to make healthier choices that support their recovery journey.
-
Seek Professional Therapy: If disturbances in rest persist, consider exploring cognitive-behavioral therapy for insomnia (CBT-I) or Eye Movement Desensitization and Reprocessing (EMDR) to address the underlying trauma. As Dr. Philip R. Gehrman emphasizes, rest disturbances often do not resolve with general trauma-focused treatment, indicating that targeted interventions are essential. Furthermore, a trial by Raskind et al. (2018) highlighted the potential of prazosin in reducing nightmares among military veterans, suggesting pharmacological options alongside psychological therapies. Success stories from individuals who have utilized CBT-I and hypnotherapy suggest a path toward enhanced rest quality and overall well-being. Remember that you are not alone in this journey; seeking professional support can make a significant difference in managing PTSD-related insomnia. Numerous clients have recounted their experiences of how hypnotherapy has not only reduced their anxiety but also enabled them to regain their rest and overall life satisfaction.
Understanding the Mechanisms Behind PTSD and Sleep Disturbances
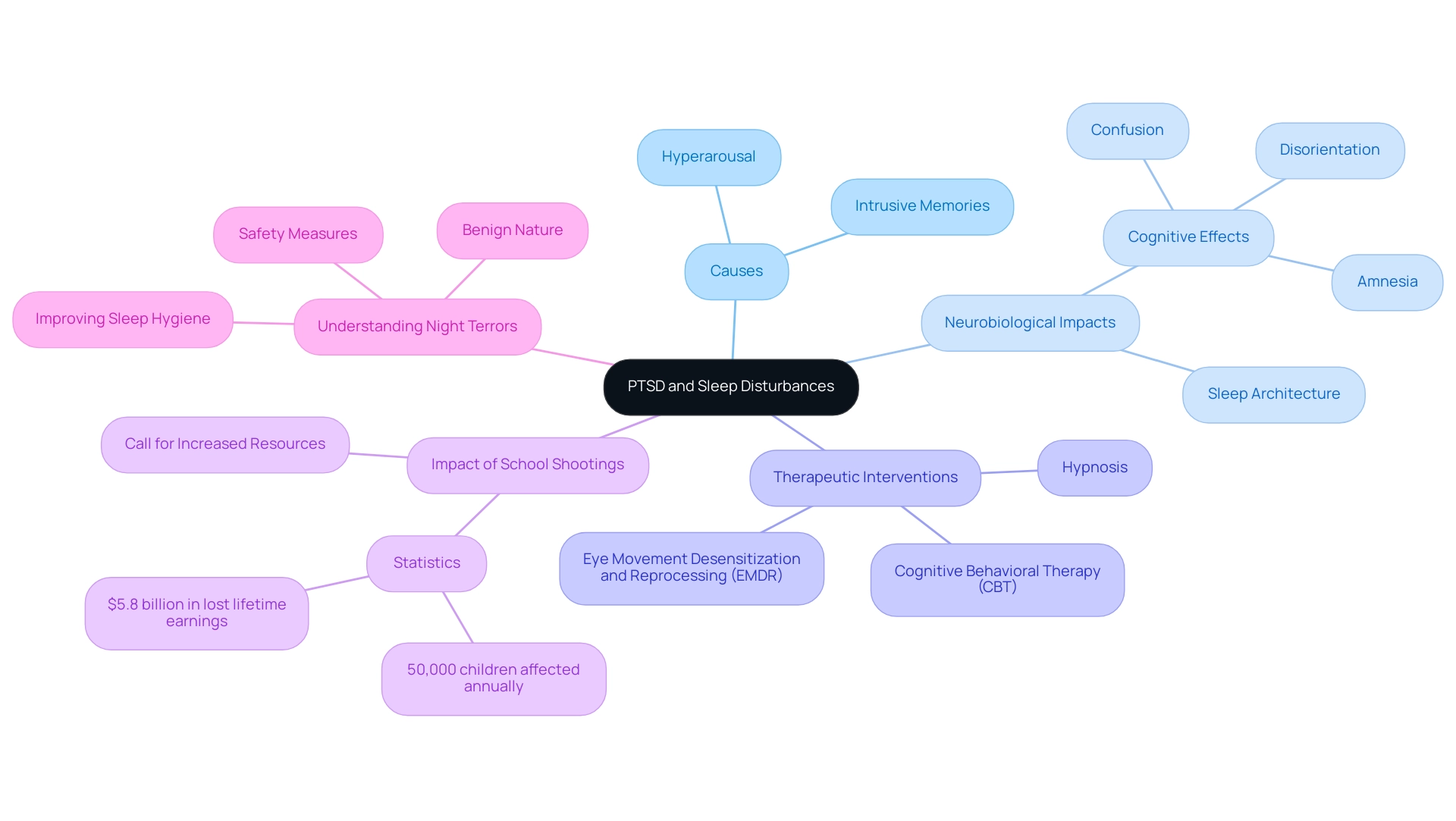
Post-traumatic stress condition significantly affects rest through multiple interconnected processes, frequently causing individuals to feel ensnared in a cycle of anguish. Approximately 50,000 children annually endure shootings at their schools, resulting in considerable mental health difficulties, including disturbances related to post-traumatic stress.
One significant factor is hyperarousal, a common symptom of PTSD that amplifies the body's stress response. This heightened state can lead to an increased heart rate and overwhelming tension, making it challenging to relax and fall asleep. Furthermore, intrusive memories of trauma may surface at night, manifesting as nightmares or night terrors that further disrupt sleep quality.
Neuroscientific research indicates that trauma can lead to neurobiological changes that alter sleep architecture, impacting the delicate balance between rapid eye movement (REM) and non-REM sleep. These alterations may contribute to confusion, disorientation, and even amnesia upon waking, leaving people struggling to make sense of their experiences. As noted by Mary L Windle, PharmD, 'Understanding the neurobiological impacts of trauma is crucial for developing effective treatment strategies.'
Understanding these mechanisms empowers individuals to seek targeted interventions that address both PTSD and insomnia holistically. Amber's journey illustrates how she overcame debilitating flashbacks and grief after trying various therapies, including talk therapy, cognitive behavioral therapy (CBT), and EMDR, which helped to a degree but did not fully resolve her issues. It was through innovative techniques like hypnosis and NLP that she found the tools to reclaim restful nights. Similarly, clients like Vanessa and Ray have shared transformative experiences where they felt a significant reduction in anxiety and emotional pain after just a few sessions. These testimonials emphasize the life-altering effects of hypnosis in addressing the underlying trauma and enhancing rest quality.
Families must also understand that night terrors, while distressing, are benign and self-limited, as highlighted in a case study on night terrors. Implementing safety measures and enhancing rest hygiene can help reduce the frequency or severity of such events. By acknowledging the relationship between trauma and rest disruptions, people can take significant actions toward recovery and reclaiming peaceful nights. Additionally, it is important to note that stress, whether acute or chronic, can exacerbate symptoms of trauma, making effective stress management strategies essential for recovery.
Prevalence and Impact of Insomnia in PTSD Patients
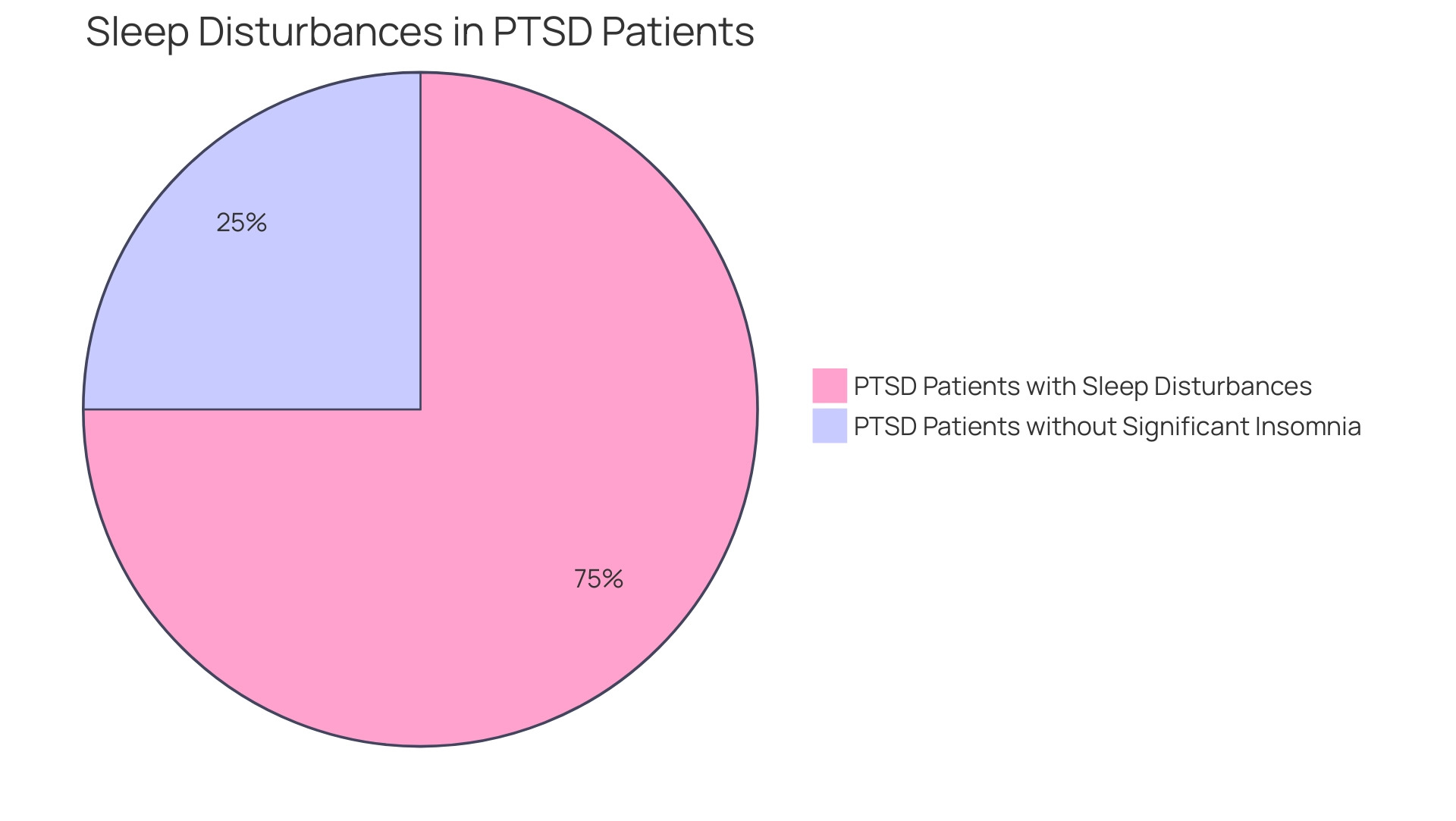
Studies show that a concerning 70% of people suffering from post-traumatic stress disorder encounter sleep issues, with sleeplessness being one of the most common and troubling signs linked to this condition. According to a 2024 study, roughly 75% of individuals with post-traumatic stress disorder indicate considerable sleep disturbances, highlighting the urgent nature of this problem.
The ramifications of insomnia extend far beyond mere tiredness; they can profoundly affect daily functioning. Individuals experiencing post-traumatic stress disorder may find themselves struggling with ongoing fatigue, irritability, and cognitive challenges, which can result in a notable decrease in their quality of life.
Dr. Jane Smith, a prominent authority in trauma recovery, states, "Insomnia can severely hinder the healing process in patients with post-traumatic stress, as restorative sleep is essential for emotional regulation and cognitive function."
Recognizing sleeplessness as a significant indicator of post-traumatic stress disorder is crucial, leading to more efficient treatment approaches.
At Goodwin Hypnosis, we specialize in emotional trauma recovery through private sessions and an online program utilizing hypnosis and NLP. Through our compassionate approach, we assist clients like Amber, who overcame trauma and grief using techniques such as guided imagery and cognitive restructuring. Amber's transformative journey illustrates the profound impact of our methods.
Take the first step toward recovery. Grasping this link between sleep disturbances and post-traumatic stress disorder is a crucial step toward healing and recovery, promoting a comprehensive approach to trauma resolution customized to the distinct requirements of each person.
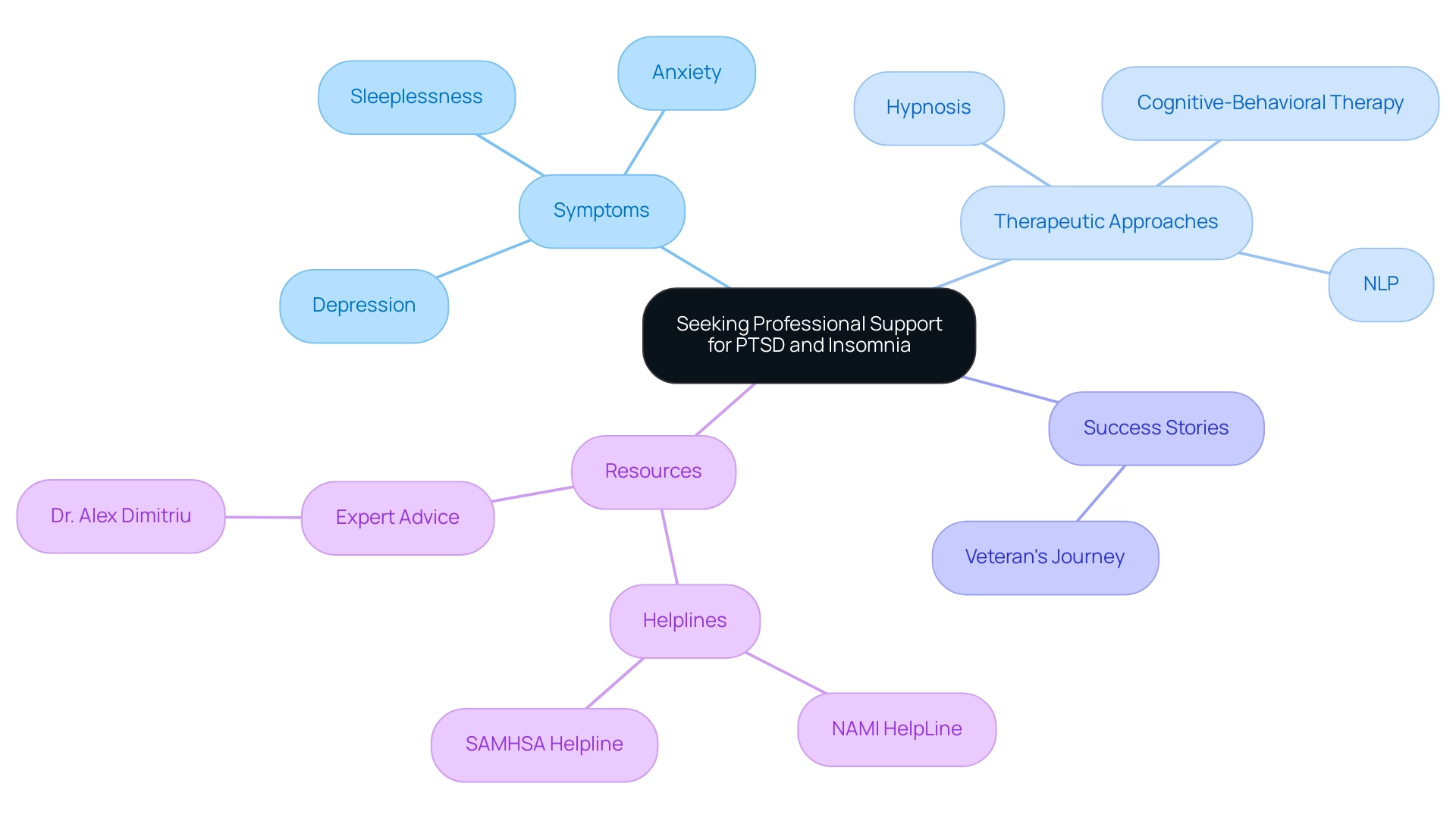
When to Seek Professional Support for PTSD and Insomnia
If you are experiencing ongoing sleeplessness that disrupts your daily life or is accompanied by significant anxiety, depression, or other symptoms of PTSD, it’s essential to consider seeking professional support. Almost 50% of people with depression also face anxiety disorders, emphasizing the interconnectedness of these conditions.
At Goodwin Hypnosis, we specialize in personalized one-on-one sessions that target the root causes of emotional trauma, stress, and anxiety through effective techniques, including hypnosis and memory reconsolidation. Many individuals have found success even after doing cognitive-behavioral therapy, which has been shown to significantly reduce PTSD-related insomnia for some patients.
Furthermore, our creative method integrating hypnosis and NLP has assisted clients in regaining restful nights and enhancing their overall quality of life. If you've attempted self-help techniques without success, experts can provide customized interventions, such as hypnosis, recognized for their effectiveness in addressing trauma-related sleep issues. Remember, taking the step to seek help is an act of courage and a vital part of your journey towards healing.
As Dr. Alex Dimitriu, a board-certified psychiatrist, emphasizes, getting the right support is crucial to navigating these challenges. Moreover, helplines such as the NAMI HelpLine and SAMHSA helpline in the U.S. are available to provide additional support as you take this important step. Staying informed about the latest news on professional support for PTSD treatment can also empower you in your recovery journey.
Conclusion
The intricate relationship between PTSD and insomnia reveals a profound challenge that many individuals face on their journey to healing. The overwhelming statistics highlight that a significant portion of those with PTSD experience sleep disturbances, which not only disrupts their rest but also exacerbates their emotional and cognitive struggles. Understanding the mechanisms behind these challenges is crucial, as it empowers individuals to confront insomnia as an integral part of their recovery process rather than a separate issue.
Implementing effective strategies such as establishing a consistent sleep routine, creating a calming sleep environment, and practicing relaxation techniques can pave the way for improved sleep quality. Additionally, seeking professional support through targeted therapies like CBT-I, EMDR, and innovative approaches such as NLP and hypnosis can provide the necessary tools for individuals to reclaim their nights and enhance their overall well-being.
Ultimately, acknowledging the interplay between PTSD and insomnia is a vital step towards recovery. By embracing a holistic approach that addresses both the emotional and physical aspects of these conditions, individuals can embark on a transformative journey toward healing, regaining control over their sleep and, consequently, their lives. It is important to remember that seeking help is a courageous step, and support is available to guide those affected by these challenges toward a more restful and fulfilling life.




