PLEASE NOTE:
While the following article relates to your Google search, the services and methods at Goodwin Hypnosis may differ from those mentioned below. Since 2007, we have helped thousands of clients to overcome emotional and behavioral challenges when all else had failed. According to many of them (and their referring healthcare providers), our methods are faster than talk therapy, easier than willpower, and safer than medication. If you’re ready to resolve your issues, skip the article and visit the rest of our website, where you can learn about our unique approach, watch client testimonial videos, and discover how working with us one-on-one could be the solution you’ve been searching for.
We can help you with a variety of issues relating to emotional trauma. While we don't diagnose disorders like PTSD, we have helped hundreds of clients to overcome a wide range of traumatic experiences and their negative effects with methods that are more efficient and comfortable than CBT or EMDR. If you would like to learn more about working with us one-on-one to clear your trauma, click here.
Introduction
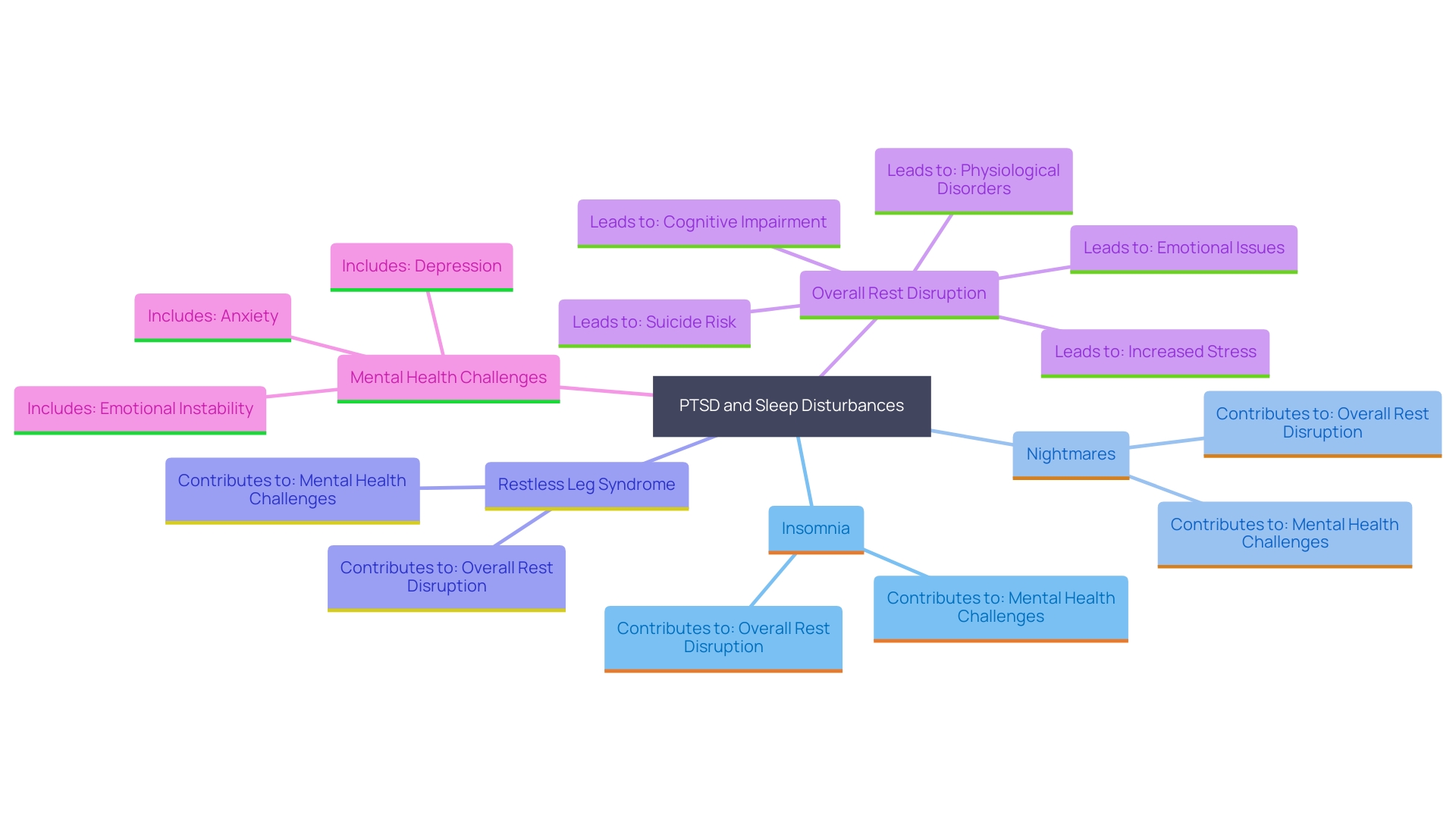
Sleep disturbances are a common and distressing issue for individuals with PTSD, often manifesting as insomnia, nightmares, and restless leg syndrome. These disruptions can severely impact sleep quality and overall well-being. Insomnia, characterized by difficulty falling or staying asleep, is prevalent among PTSD sufferers, highlighting the pervasive nature of sleep issues in this population.
Nightmares, frequently involving re-experiencing traumatic events, heighten anxiety and disrupt rest, exacerbating the already significant emotional turmoil associated with PTSD. Additionally, sleep apnea and periodic limb movements further fragment sleep, making restful nights elusive. Understanding and addressing these sleep disturbances is essential, as improved sleep can significantly enhance mental health and daily functioning for those affected by PTSD.
Common Sleep Disturbances in PTSD
People with post-traumatic stress often experience a variety of rest issues, including insomnia, nightmares, and restless leg syndrome. Insomnia is a common manifestation, characterized by difficulty falling asleep, staying asleep, or waking up prematurely. In a study involving 211 adults with chronic insomnia, persistent rest issues were noted despite adequate rest opportunities, highlighting the pervasive nature of insomnia among those with PTSD. Nightmares, frequently a re-experiencing of traumatic events, can lead to heightened anxiety and fear, severely affecting rest quality. A study involving 419 individuals with narcolepsy found an 85.8% prevalence rate of nightmares, illustrating the significant overlap between parasomnias and PTSD-related disturbances during rest. The pressure and psychological distress linked to post-traumatic stress disorder likely worsen these nightmares, contributing to overall rest disruption and daytime impairment. Furthermore, a significant occurrence of breathing disruptions during slumber and intermittent limb movements has been noted in individuals with post-traumatic stress disorder, further contributing to disrupted and decreased duration of rest. Tackling these rest disturbances is essential, as enhancing rest quality can greatly improve overall mental well-being and daily functioning.
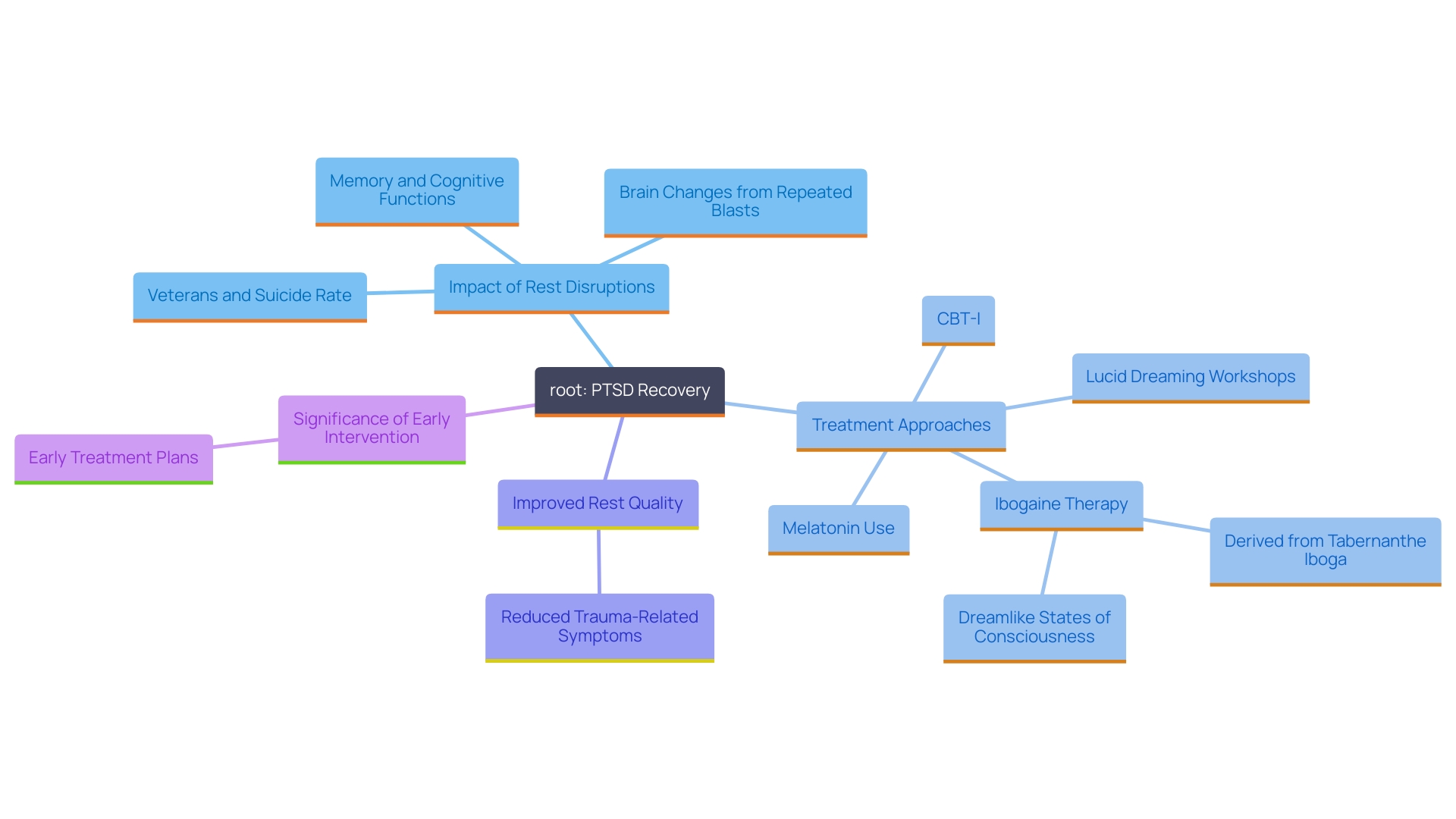
The Impact of Sleep Disturbances on PTSD Symptoms
Sleep disturbances can significantly exacerbate PTSD symptoms, leading to heightened emotional distress, irritability, and difficulty concentrating. When rest is compromised, the brain struggles to process and integrate traumatic memories, which can perpetuate the cycle of anxiety and hyperarousal. This deficiency of restorative rest can also impair overall functioning, making it challenging for individuals to engage in daily activities or therapeutic interventions.
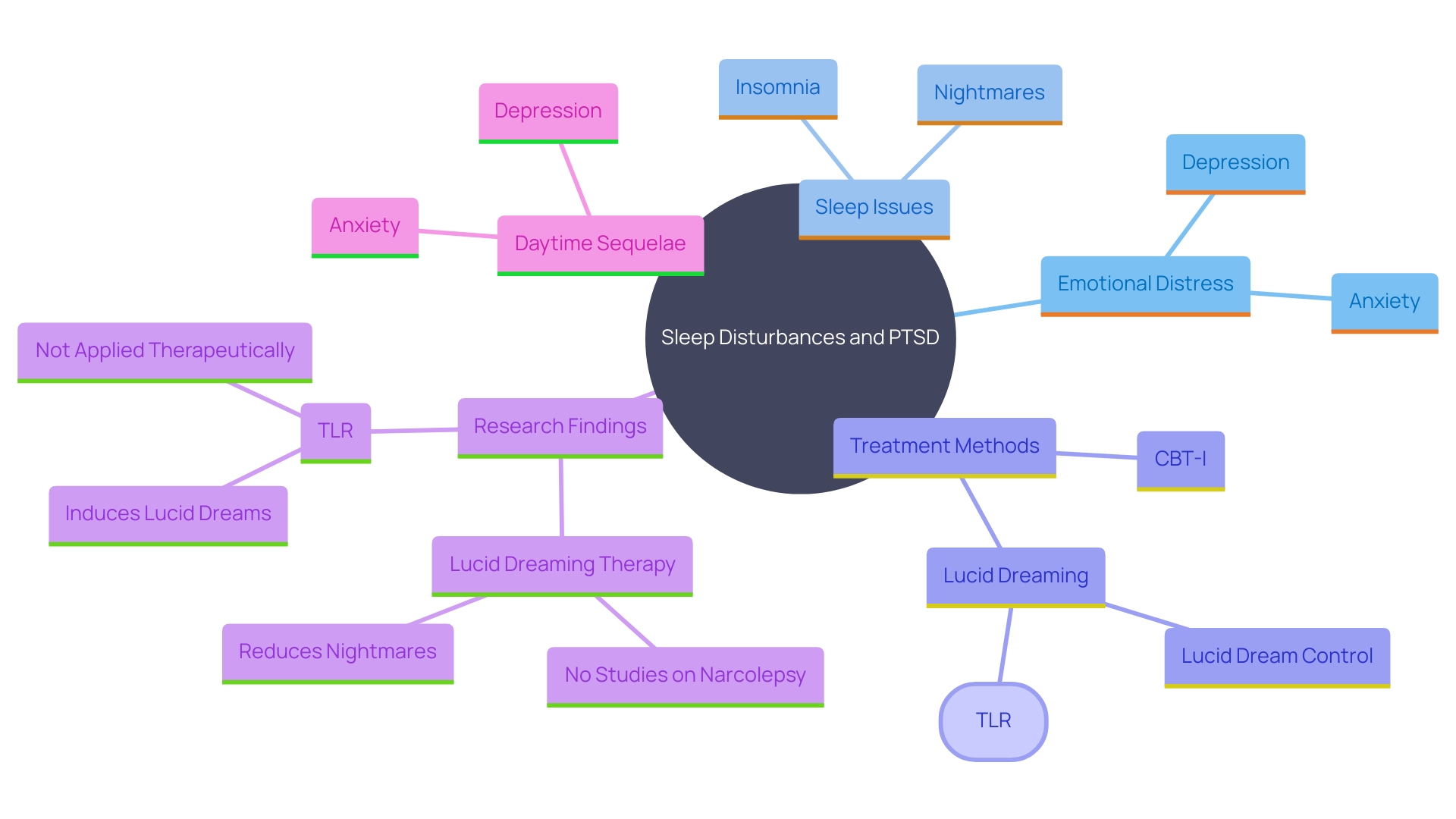
Research has indicated a significant occurrence of sleep apnea and periodic limb movements among individuals with post-traumatic stress disorder, further contributing to disturbances in rest and decreased duration of rest. This link between rest problems and post-traumatic stress disorder emphasizes the significance of tackling rest concerns as an element of a thorough treatment strategy. For example, a study involving a six-day lucid dreaming workshop showcased the potential of applying lucid dreaming techniques to change nightmares and incorporate trauma, providing a unique method to enhance rest quality in PTSD patients.
Furthermore, recent studies have highlighted the substantial effect of anxiety on sleeping problems. Anxiety-related psychopathology is often linked to feelings of uncertainty and insecurity, which can severely disrupt rest patterns. This disruption can appear as insomnia, nightmares, or other disturbances during rest, worsening trauma-related symptoms and overall mental well-being. Addressing these anxiety-related rest issues is crucial, as prolonged rest problems can impair cognitive function, increase stress, and even elevate suicide risk.
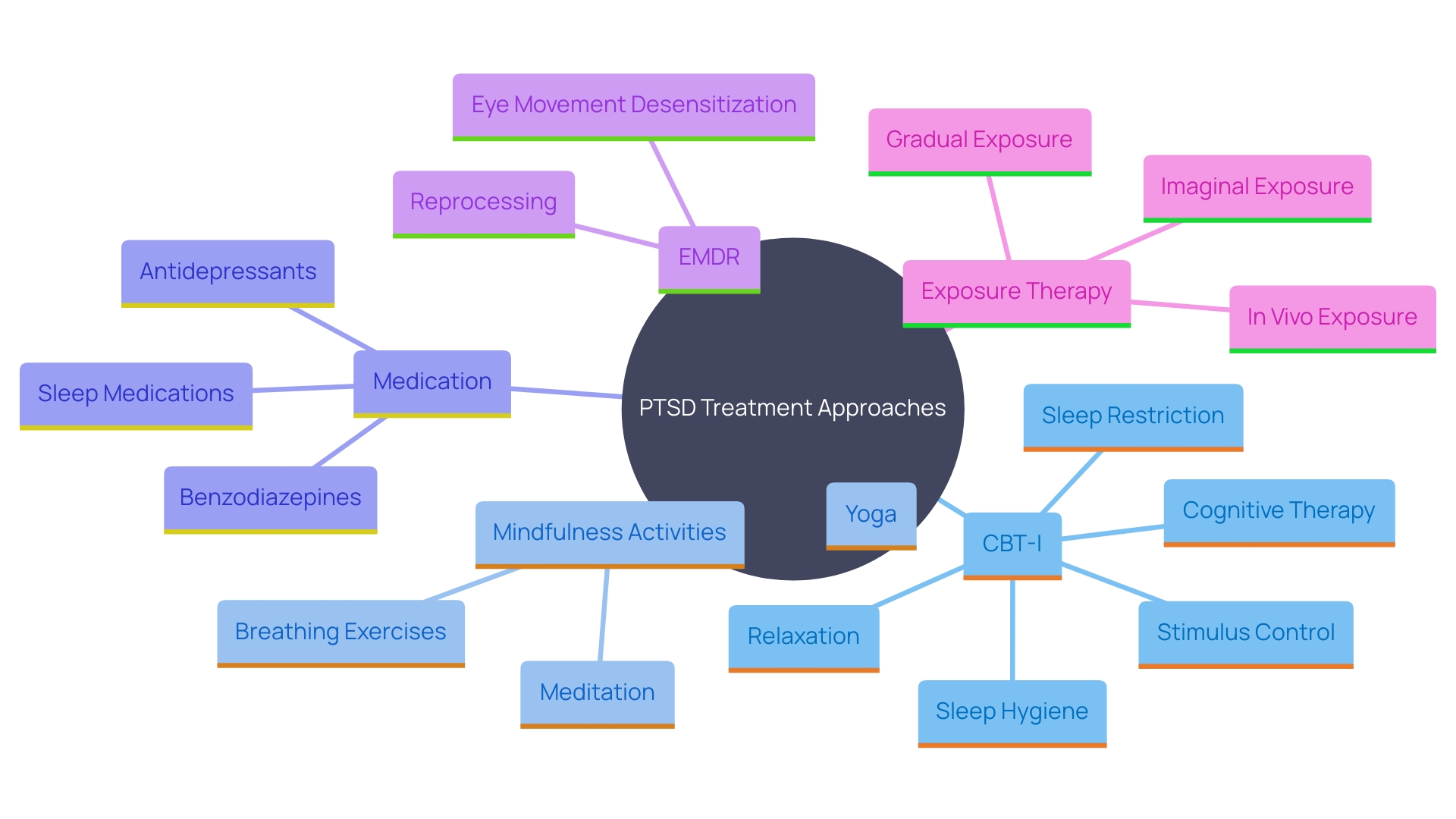
Successful measures for disruptions in rest associated with trauma may involve cognitive-behavioral therapy for insomnia (CBT-I), which has been demonstrated to enhance rest standards and lessen trauma-related symptoms. Additionally, medications like prazosin have been found to help alleviate nightmares, while non-pharmacological approaches such as mindfulness and relaxation techniques can also be beneficial. Grasping and tackling the complex connection between rest disruptions and post-traumatic stress disorder is crucial for promoting recovery and improving the quality of life for those impacted by this condition.
Mechanisms Linking Sleep Disturbances and PTSD
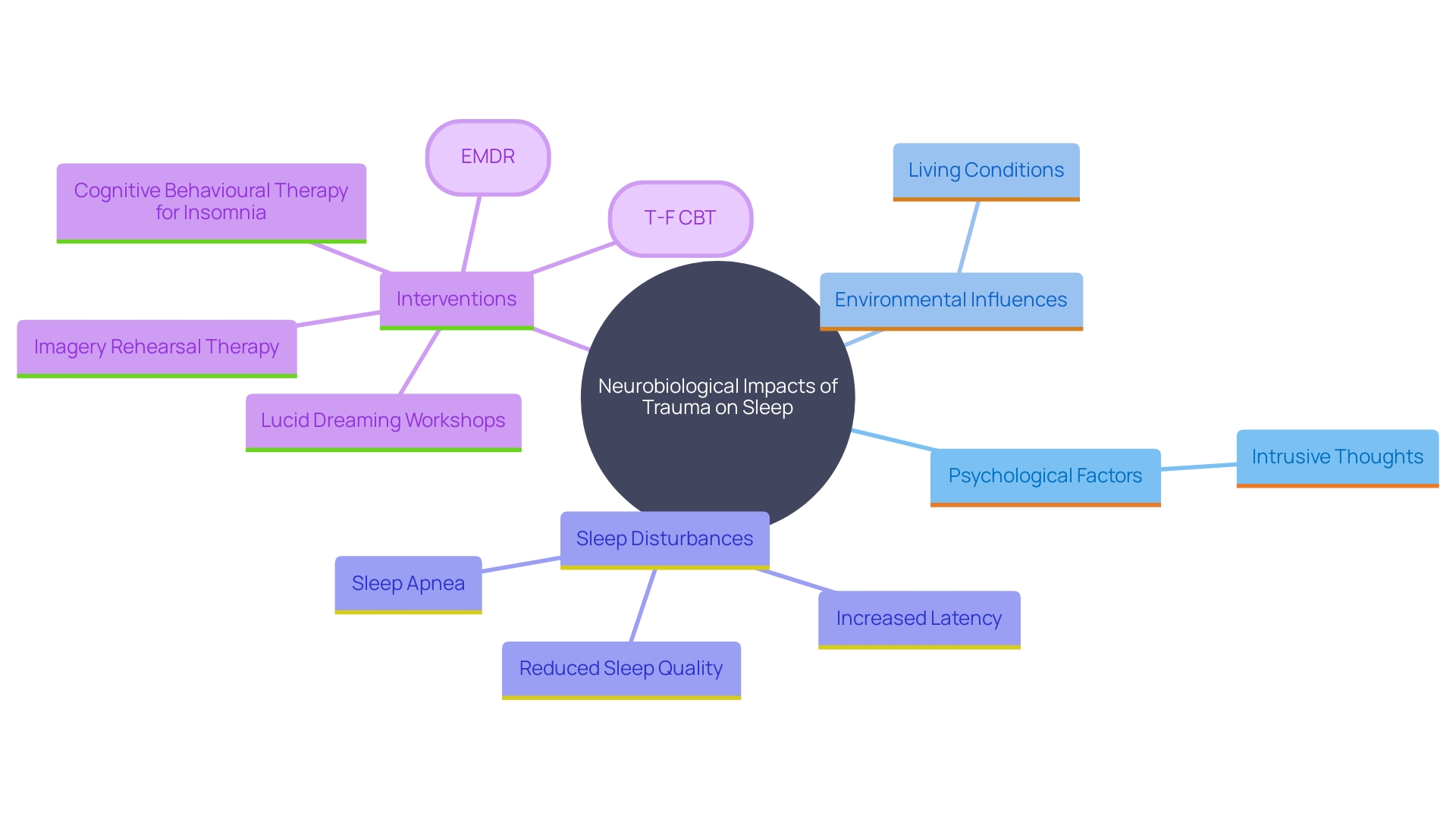
The complex connection between rest disruptions and post-traumatic stress disorder includes neurobiological, psychological, and environmental elements. Trauma can interfere with the brain's rest-activity cycle, hindering the control of neurotransmitters essential for rest. This disruption frequently appears as hyperarousal, a typical symptom of trauma that increases alertness and obstructs relaxation and the onset of rest. Psychological factors, including persistent, intrusive thoughts about the trauma, exacerbate these rest difficulties.
Research emphasizes the considerable reduction in rest standards among PTSD patients in comparison to healthy controls. These individuals often experience poorer subjective rest quality, increased latency in rest, reduced duration of rest, and efficiency, alongside a higher frequency and severity of nightmares. Polysomnography (PSG) assessments confirm these findings, showing reduced rest efficiency, more awakenings, longer REM duration latency, and increased wakefulness during the night.
Research also indicates that individuals with trauma-related conditions may encounter disorders associated with rest, such as apnea during rest and periodic limb movements, further interrupting rest continuity and decreasing total rest duration. Creative methods, like lucid dreaming workshops, have demonstrated potential in assisting individuals with trauma to change their nightmares and assimilate their experiences, as indicated by notable enhancements in symptom scales after such interventions.
The neurobiological underpinnings of these disturbances are equally compelling. Research involving mice has demonstrated that stress-induced activation of specific neurons in the hypothalamus can fragment rest, further elucidating the complex interplay between stress and rest disorders. Comprehending these processes is vital for creating successful treatments that can bring back restorative rest and improve general wellness for individuals struggling with post-traumatic stress disorder.
Treatment Options for Sleep Disturbances in PTSD
Addressing disturbances in PTSD often requires a multi-faceted approach. Cognitive-behavioral therapy for insomnia (CBT-I) is an effective approach that addresses the thoughts and behaviors contributing to rest problems. Results have indicated considerable enhancements in rest condition, with average ratings rising from 6.44 to 8.55 (p = 0.005), and decreases in insomnia intensity. 'Furthermore, mindfulness activities and relaxation methods, including hatha yoga and daily mindfulness exercises, have been demonstrated to positively influence mental well-being and restfulness in high-stress professions.'.
Medication may also be utilized to enhance rest quality, but recent research emphasizes novel methods such as recollection reactivation during slumber. In a study, participants underwent a session of EMDR prior to resting, where they were directed through their traumatic experiences with lateral eye movements and auditory clicks. These auditory signals were then utilized for recalling information during specific phases of slow-wave rest, a crucial stage for information consolidation. This method demonstrated encouraging outcomes in alleviating trauma-related symptoms by improving cognitive processing during slumber.
Moreover, exposure therapy can be beneficial for processing traumatic experiences, which indirectly alleviates sleep-related problems. Regular nightmares impact up to 70% of individuals with post-traumatic stress disorder, and unsettling dreams can have significant effects on emotional and physical well-being. By confronting these distressing memories through therapy, it is possible to decrease the frequency of nightmares and enhance overall rest.
The Importance of Early Identification and Treatment of Sleep Disturbances
Identifying and tackling rest disruptions early in the management of post-traumatic stress disorder is essential for successful recovery. A study involving a six-day lucid dreaming workshop for individuals with chronic post-traumatic stress disorder demonstrated that targeted interventions can significantly enhance rest quality and reduce trauma-related symptoms. Participants reported better management of nightmares and trauma integration, highlighting the importance of early intervention. Furthermore, studies indicate that rest disorders such as apnea and periodic limb movements are common in PTSD patients, leading to decreased duration of rest and frequent awakenings.
Initial treatment approaches, like emphasizing rest hygiene and introducing melatonin, have demonstrated potential in lowering the likelihood of self-injury and enhancing overall wellness. For instance, a study involving adolescents struggling with mental health issues found that melatonin helped mitigate suicidal thoughts and behaviors, underlining the potential benefits of sleep-focused interventions. Moreover, supportive psychotherapy has been shown to improve rest conditions and decrease anxiety, with statistical evaluations indicating notable advancements in insomnia severity ratings.
Including rest evaluations and interventions as part of PTSD treatment plans is essential. Specialists such as Ana Imia Fins, Ph.D., highlight the importance of disturbances in rest in worsening aggressive behaviors and suggest particular methods to improve rest standards. These include cognitive-behavioral therapy for insomnia (CBT-I) and other behavioral rest medicine interventions. By tackling rest problems promptly, individuals with post-traumatic stress disorder can achieve a quicker restoration of emotional and mental stability, ultimately enhancing their overall standard of living.
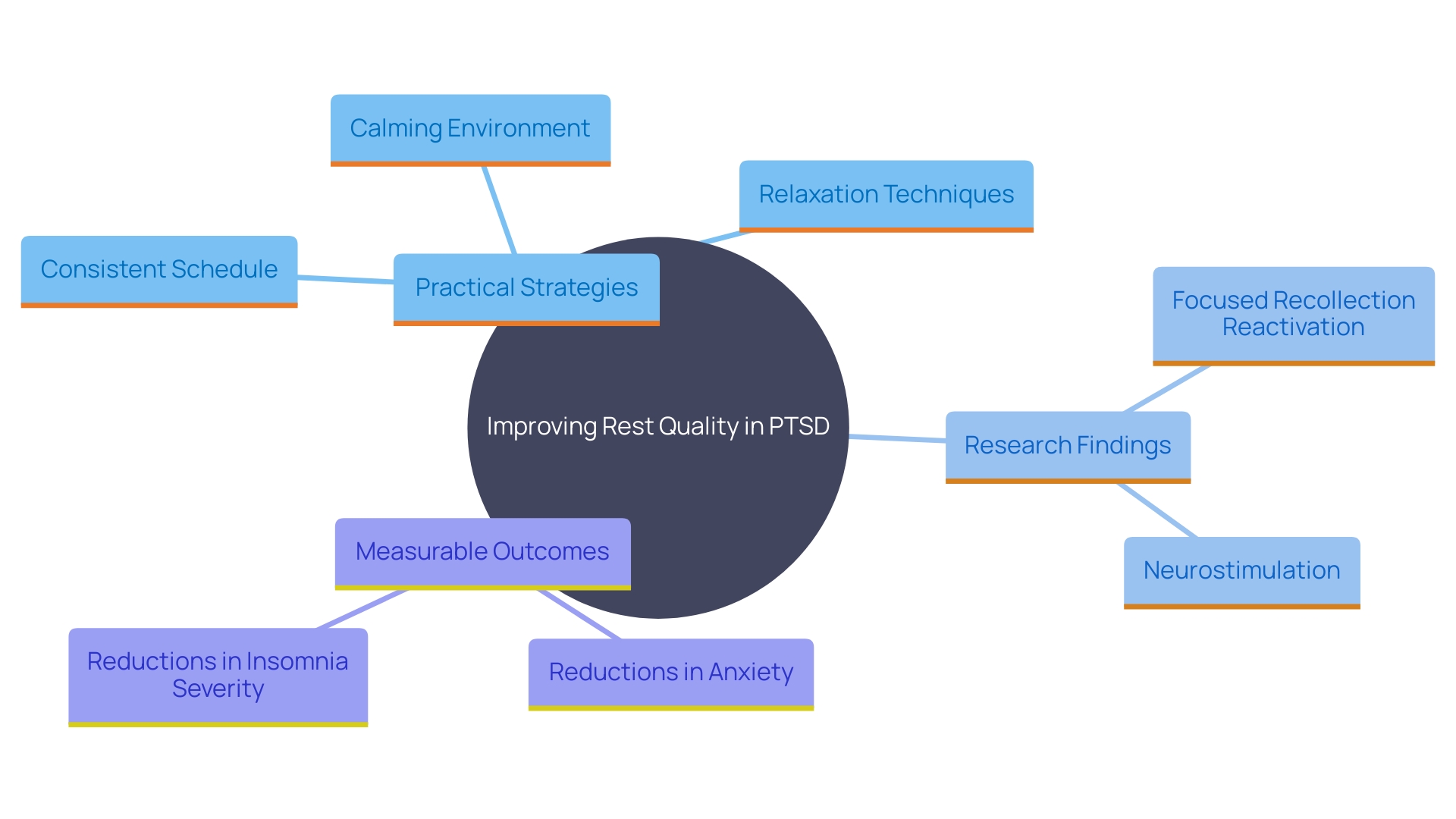
Practical Tips for Improving Sleep in PTSD Patients
Applying practical strategies can significantly improve rest quality for those with PTSD. Maintaining a consistent rest schedule and creating a calming bedtime routine are essential. Ensuring a comfortable resting environment by adjusting lighting, temperature, and noise levels can also make a substantial difference. Reducing screen time prior to going to bed and steering clear of caffeine and large meals in the evening are essential measures to encourage improved rest. These practices align with findings that highlight the brain's unique activity during rest, where it replays and processes memories, reducing their emotional impact.
Engaging in relaxation techniques, such as deep breathing or meditation, can further enhance the ability to unwind and prepare for rest. This is backed by studies indicating that heart rate can be influenced by auditory stimuli during rest, and calming words heard while resting can decrease cardiac activity. Such findings highlight the significance of establishing a calming atmosphere favorable for rest.
Furthermore, focused recollection reactivation (TMR) has demonstrated potential in enhancing trauma-related symptoms. In a study involving 33 PTSD patients, researchers used neurostimulation to time recollection reactivation signals with specific phases of slow-wave rest, a stage crucial for consolidation of information. This method significantly enhanced the therapeutic effects of eye movement desensitization and reprocessing (EMDR), demonstrating that integrating new memories into existing networks can reduce their emotional impact.
Data backs these methods, demonstrating notable enhancements in rest standards and decreases in anxiety and insomnia intensity with supportive psychotherapy. For example, anxiety levels reduced from an average score of 4.49 to 2.65, and insomnia severity ratings enhanced across all factors, with rest condition reflecting an average score increase from 6.44 to 8.55.
In summary, combining these practical strategies with insights from recent research can create a comprehensive approach to improving sleep quality for those with PTSD.
Conclusion
Sleep disturbances are a significant challenge for individuals living with PTSD, manifesting as insomnia, nightmares, and other sleep-related issues. These disturbances not only disrupt the quality of sleep but also exacerbate PTSD symptoms, leading to heightened emotional distress and impairing daily functioning. The intricate relationship between sleep and PTSD underscores the urgency in addressing these issues as part of a holistic treatment approach.
Recognizing the importance of early identification and intervention is crucial in fostering recovery. Effective strategies, such as cognitive-behavioral therapy for insomnia, mindfulness practices, and innovative techniques like targeted memory reactivation, show promise in improving sleep quality and alleviating PTSD symptoms. These interventions can significantly enhance an individual's ability to manage trauma and improve overall well-being.
Practical tips for improving sleep, including maintaining a consistent sleep schedule, creating a calming bedtime routine, and engaging in relaxation techniques, can be beneficial. Implementing these strategies not only aids in better sleep but also contributes to emotional stability and resilience. By prioritizing sleep as an integral component of PTSD treatment, individuals can embark on a path toward healing and regain a sense of balance in their lives.




