PLEASE NOTE:
While the following article relates to your Google search, the services and methods at Goodwin Hypnosis may differ from those mentioned below. Since 2007, we have helped thousands of clients to overcome emotional and behavioral challenges when all else had failed. According to many of them (and their referring healthcare providers), our methods are faster than talk therapy, easier than willpower, and safer than medication. If you’re ready to resolve your issues, skip the article and visit the rest of our website, where you can learn about our unique approach, watch client testimonial videos, and discover how working with us one-on-one could be the solution you’ve been searching for.
We can help you with a variety of issues relating to emotional trauma. While we don't diagnose disorders like PTSD, we have helped hundreds of clients to overcome a wide range of traumatic experiences and their negative effects with methods that are more efficient and comfortable than CBT or EMDR. If you would like to learn more about working with us one-on-one to clear your trauma, click here.
Introduction
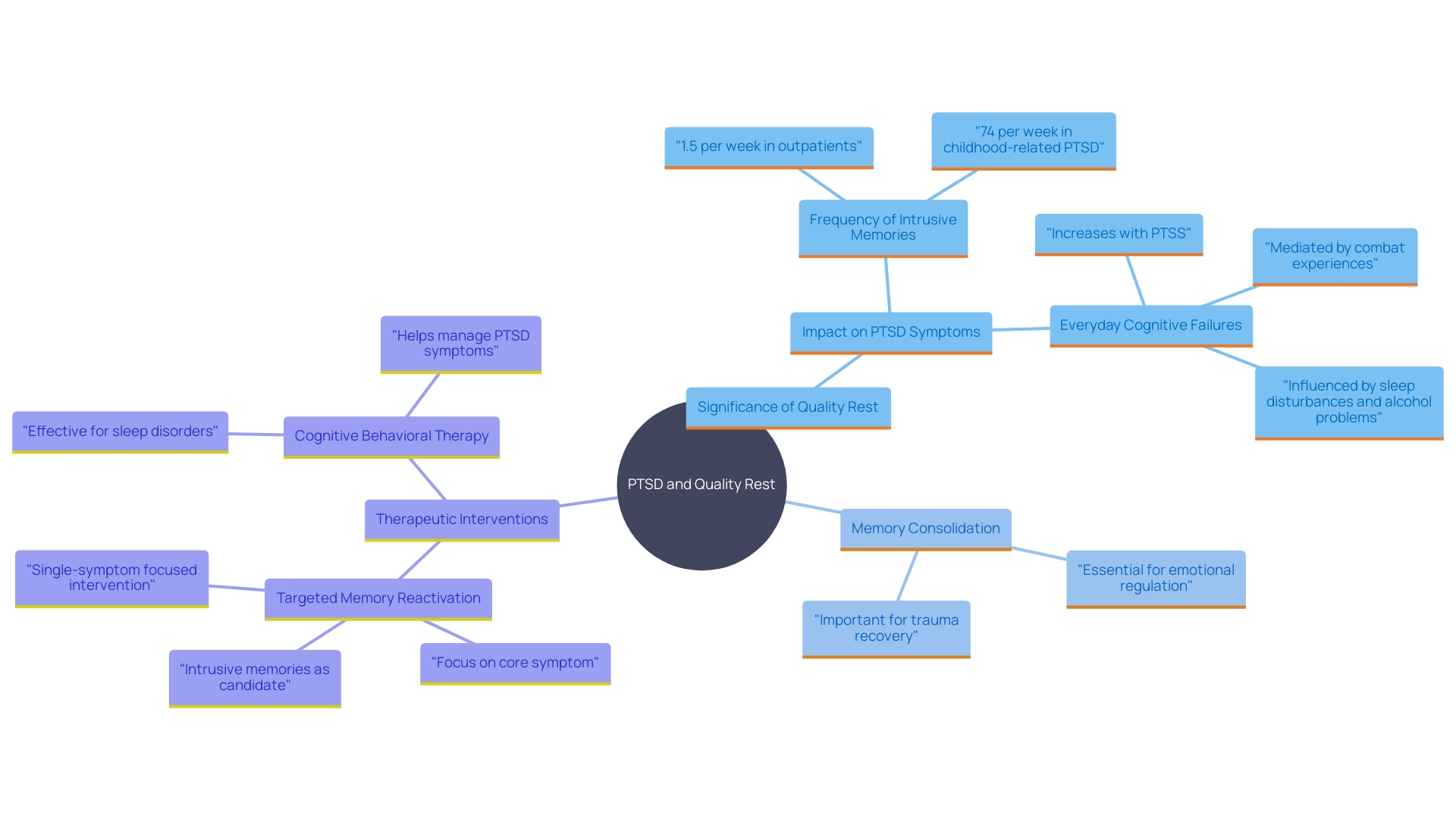
Sleep is a cornerstone of mental health, playing an especially crucial role in the recovery process for those grappling with PTSD. When the brain receives restorative sleep, it has the opportunity to process emotions and experiences, a process known as memory consolidation. This integration is essential for reducing the emotional impact of traumatic memories.
However, sleep disturbances, such as insomnia, sleep apnea, and periodic limb movements, are prevalent among individuals with PTSD, often exacerbating their symptoms and hindering recovery.
The connection between sleep and stress is significant; poor sleep can amplify stress levels, creating a vicious cycle that makes healing even more challenging. Research underscores the importance of quality sleep in regulating mood, enhancing cognitive function, and fostering emotional resilience. Innovative approaches, like targeted memory reactivation during sleep, have shown promise in enhancing the therapeutic effects of PTSD treatments.
By prioritizing sleep health and adopting holistic treatment strategies, individuals with PTSD can improve their overall well-being and progress more effectively on their path to recovery.
Why Sleep is Important for PTSD Recovery
Rest is an essential part of mental well-being, particularly for those healing from trauma. Quality rest enables the brain to process emotions and experiences, which is essential for healing. This process, known as memory consolidation, is crucial for integrating new memories into existing networks and reducing their emotional impact. Regrettably, disruptions in rest are frequent among individuals with post-traumatic stress disorder, with a high occurrence of apnea during slumber and periodic limb movements that interrupt rest. As per a study, insomnia can deteriorate mental and physical well-being, and individuals with post-traumatic stress often indicate challenges in sleeping at least one night each week.
When rest is compromised, it can exacerbate PTSD symptoms, making recovery more challenging. For instance, the American Psychological Association found that 21% of adults reported increased stress levels when they weren't obtaining sufficient rest. Moreover, 45% of individuals with increased stress levels reported that inadequate rest exacerbated their stress. This highlights the importance of restorative rest in regulating mood, enhancing cognitive function, and fostering emotional resilience—essential for those grappling with the impacts of trauma.
Research has shown that targeted memory reactivation (TMR) during rest can strengthen the therapeutic effects of treatments like EMDR for PTSD patients. This approach utilizes the brain's unique activity during rest to reprocess traumatic memories more effectively. The Centers for Disease Control and Prevention also emphasize that lack of rest makes individuals 2.5 times more likely to experience mental distress. Therefore, ensuring quality rest is not just advantageous but essential for mental well-being and healing from trauma.
In addressing sleep disturbances, holistic approaches are recommended. For instance, cognitive behavioral therapy for sleep disorders (CBT-I) has been demonstrated to enhance emotional brain responsiveness and resilience in individuals with sleep difficulties. This is essential as sleeplessness is a significant risk factor for developing depressive disorders. By prioritizing rest wellness and integrating comprehensive treatment strategies, individuals with post-traumatic stress can better manage their symptoms and enhance their overall well-being.
How PTSD Affects Sleep
PTSD can profoundly disrupt rest, causing nightmares, hypervigilance, and insomnia. The constant state of alertness makes it challenging to relax and fall asleep. Fear of reliving traumatic experiences in dreams often results in avoiding rest, creating a cycle of deprivation and heightened anxiety. Research emphasizes the brain's activity during rest as it processes and consolidates memories, which is crucial for reducing their emotional impact. A recent study applied targeted memory reactivation (TMR) to individuals with post-traumatic stress disorder, aiming to enhance the therapeutic effects of eye movement desensitization and reprocessing (EMDR). This involved using memory reactivation cues during specific phases of slow-wave rest. Results indicated considerable enhancements in trauma-related symptoms, rest quality, and anxiety reduction. Another study showed that lucid dreaming methods might assist participants in managing their nightmares and incorporating trauma, resulting in reduced symptoms of post-traumatic stress. Tackling issues related to rest is crucial, as better slumber can boost stress resilience and overall health.
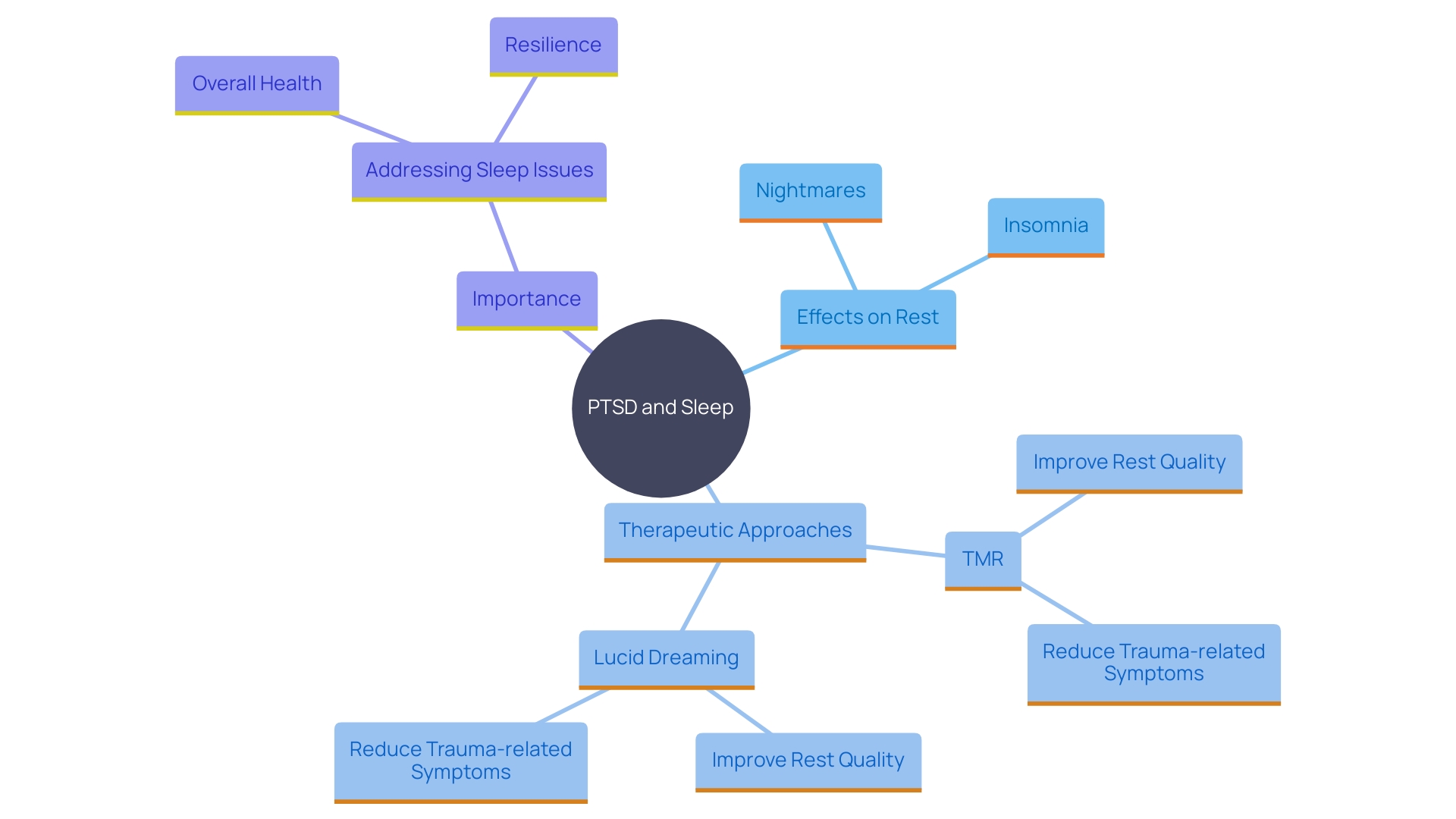
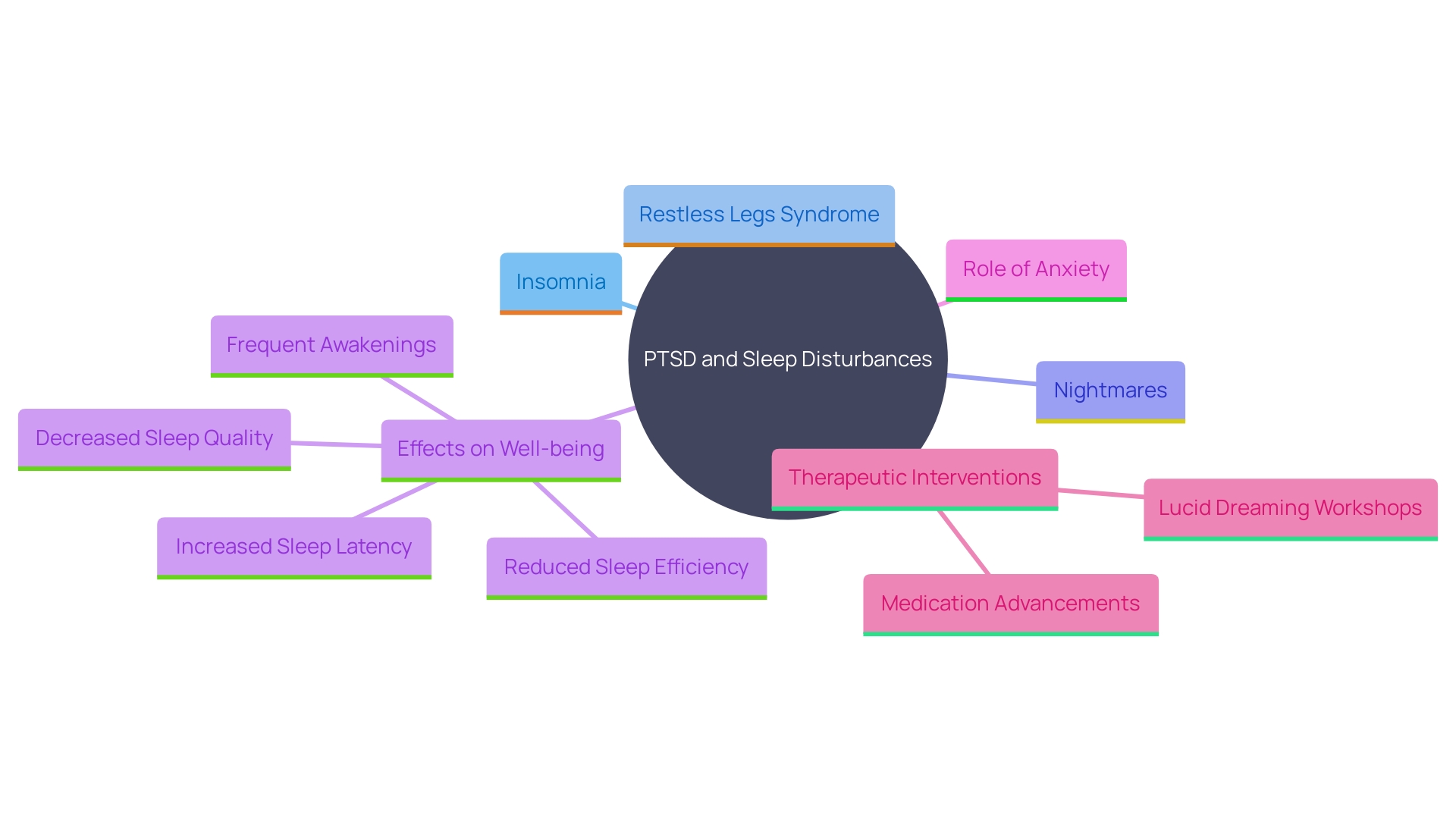
Common Sleep Problems in PTSD
People with post-traumatic stress often encounter various forms of nighttime disruptions, such as difficulty falling asleep, restless legs syndrome, and breathing interruptions during rest. Insomnia is characterized by difficulty falling or staying asleep, while nightmares can lead to frequent awakenings. Restless legs syndrome can cause uncomfortable sensations in the legs, disrupting the ability to fall asleep. These issues can collectively contribute to chronic fatigue and decreased overall well-being. A study conducted over a six-day lucid dreaming workshop found that participants with chronic post-traumatic stress disorder who practiced lucid dreaming techniques experienced significant improvements in their ability to transform nightmares and integrate trauma. Statistical analyses revealed that supportive psychotherapy significantly improved outcomes, with decreased anxiety levels and reduced insomnia severity scores, showing an increase in overall rest quality. 'Additionally, studies show that anxiety, a frequent co-occurrence with post-traumatic stress disorder, worsens issues related to rest, emphasizing the necessity for focused strategies that tackle both anxiety and problems with rest. Encouraging advancements in medication, like tirzepatide, have also demonstrated significant enhancements in apnea, providing optimism for more efficient therapies that tackle various signs of PTSD-related slumber issues.
Non-Pharmacological Interventions for Sleep Disturbances in PTSD
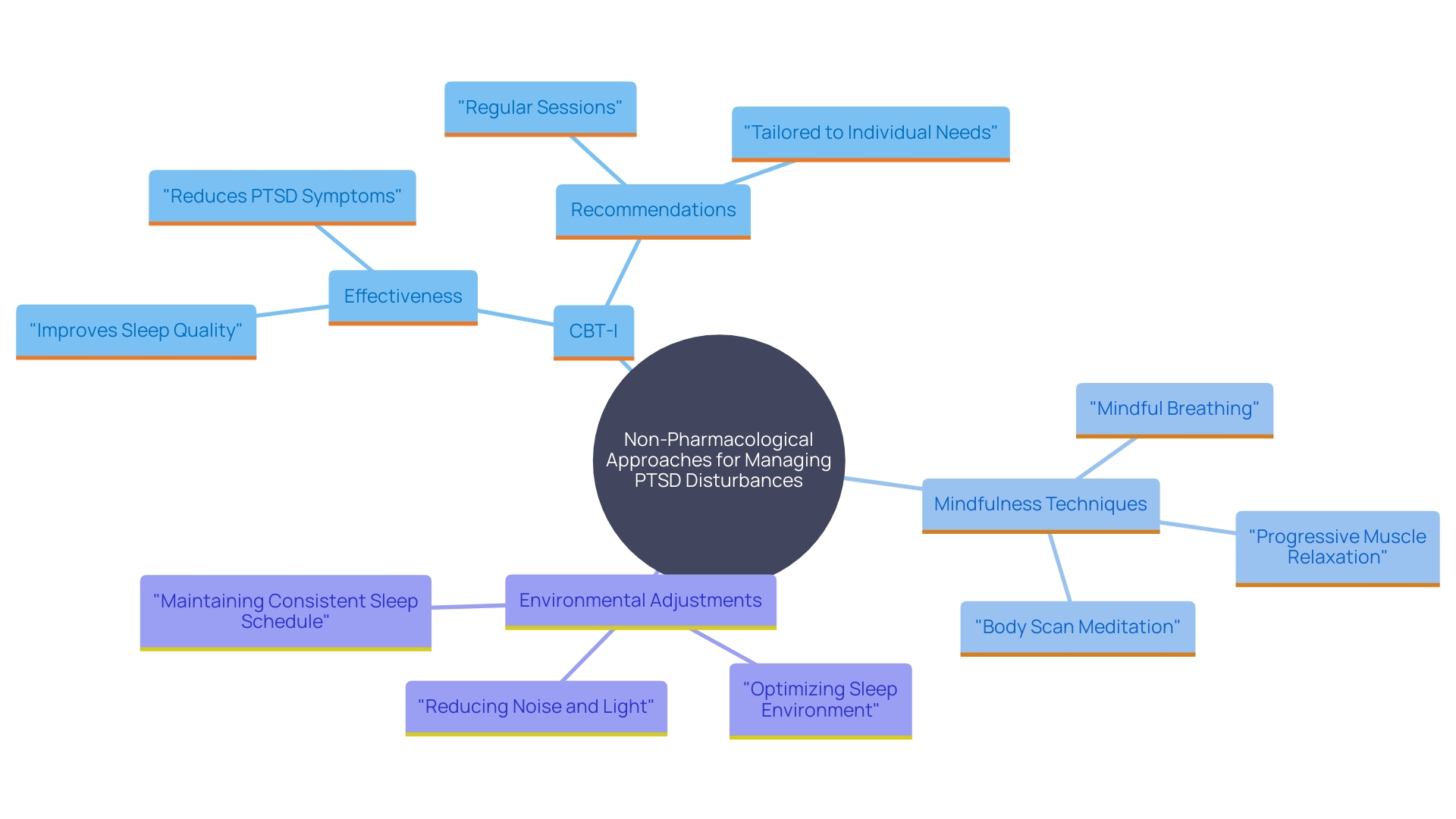
Addressing disturbances related to PTSD can benefit significantly from various non-pharmacological approaches. Cognitive Behavioral Therapy for Insomnia (CBT-I) is a comprehensive, structured program that has demonstrated effectiveness in both clinical studies and practical application. This therapy assists individuals in recognizing and modifying the thoughts and behaviors that lead to their rest issues. For example, the Netherlands Sleep Registry discovered that CBT-I resulted in considerable enhancements in rest quality, lowering disturbance severity scores and improving overall rest quality (mean score: 6.44 to 8.55, p = 0.005). Additionally, CBT-I is recommended by the American College of Physicians and the US Department of Veteran’s Affairs as the first-line therapy for chronic insomnia.
Mindfulness and relaxation techniques, such as meditation and deep breathing exercises, are also beneficial. A study by the University of South Florida demonstrated that mindfulness-based stress reduction programs could enhance rest, reduce stress, and improve overall health among participants. Nurses involved in the study reported improved rest quality after engaging in mindfulness practices, highlighting the importance of staying present and reducing fixation on negative thoughts.
Setting up a regular rest schedule and developing a conducive atmosphere are essential measures in enhancing rest quality. Consistent routines help regulate the body's internal clock, making it easier to fall asleep and wake up at the same time every day. Creating a sleep-friendly environment involves reducing noise and light, keeping the bedroom cool, and ensuring a comfortable mattress and pillows. These adjustments can make a significant difference in promoting restful and uninterrupted rest.
In general, these non-drug approaches, backed by studies and clinical proof, offer useful resources for individuals aiming to handle issues related to post-traumatic stress effectively.
Pharmacological Interventions for Sleep Disturbances in PTSD
For individuals facing rest issues associated with post-traumatic stress disorder, medication may be an essential component of their treatment strategy. Selective serotonin reuptake inhibitors (SSRIs), such as fluvoxamine, sertraline, or paroxetine, are often the first-choice medications for alleviating PTSD symptoms and improving sleep quality. However, their effectiveness in addressing sleep disturbances and nightmares can be limited, necessitating the use of additional sleep-inducing drugs or atypical antipsychotics. For example, prazosin has demonstrated effectiveness in decreasing nightmares and hyperarousal.
Benzodiazepines and other aids for resting may be prescribed for short-term relief, but their long-term use is generally not recommended due to the risk of dependency and side effects. Cognitive-behavioral therapy for insomnia (CBT-I) is often recommended as the first-line treatment for chronic insomnia, either alone or in combination with pharmacological interventions.
It's essential for individuals to work closely with their healthcare providers to find the right balance of medications and therapies, monitoring for potential side effects and making adjustments as needed. The goal is to optimize treatment efficacy while minimizing the risk of polypharmacy and its associated complications.
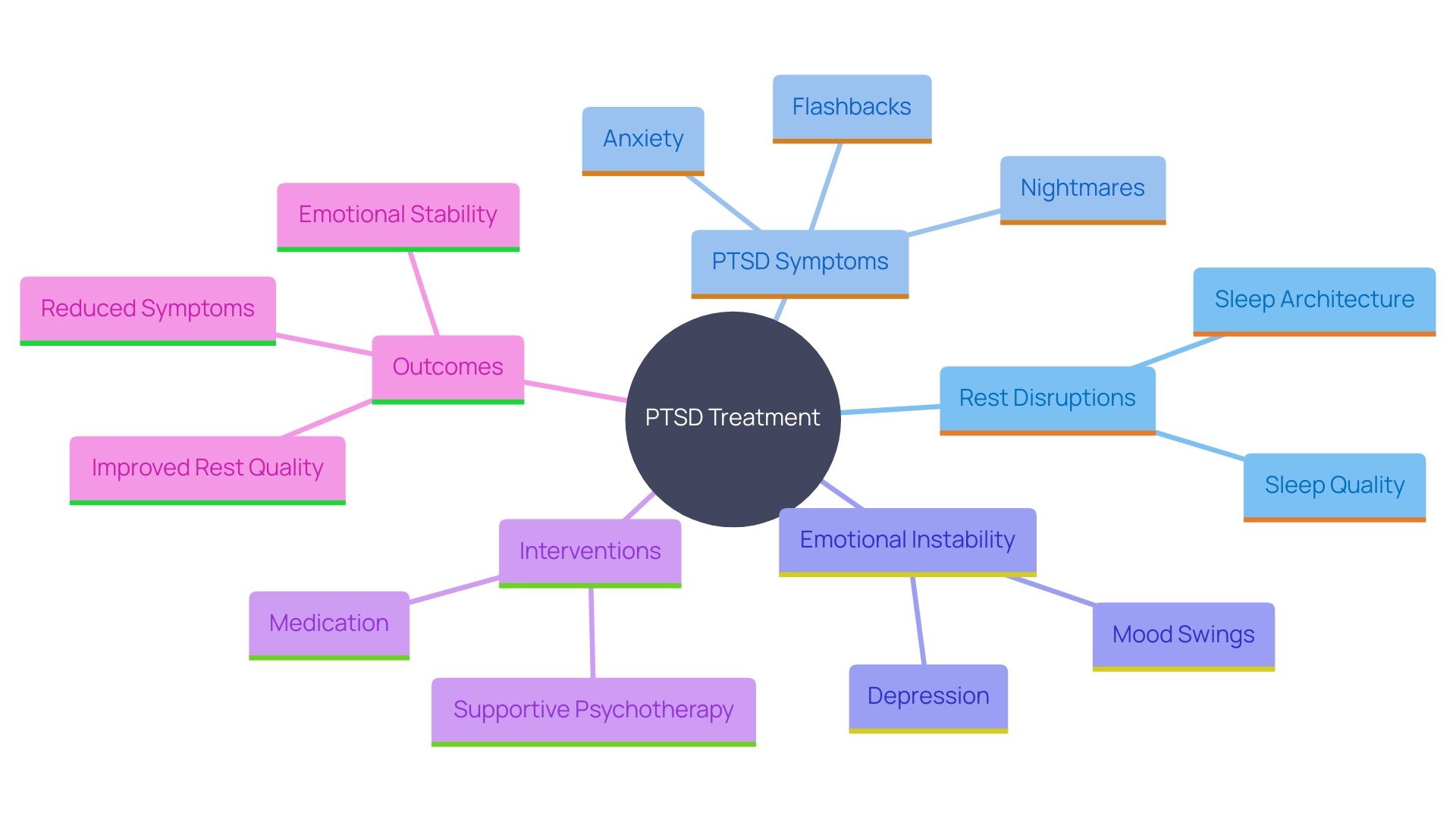
Impact of Sleep Disturbances on PTSD Outcomes
The connection between rest disruptions and post-traumatic stress disorder results is significant. Inadequate rest can worsen PTSD symptoms, resulting in increased emotional instability and challenges in managing daily activities. Research has indicated that interventions like supportive psychotherapy can significantly enhance rest quality, reduce insomnia severity, and decrease anxiety levels. For instance, a study utilizing statistical analyses like paired t-tests and McNemar tests found that anxiety levels in patients decreased from a mean score of 4.49 to 2.65, while quality of rest improved from a mean score of 6.44 to 8.55. These enhancements were not only statistically important but also clinically relevant, showing that addressing rest problems is essential for effective PTSD treatment. Furthermore, the bidirectional connection between rest and stress resilience highlights the significance of addressing disturbances in rest to improve overall recovery. Improved rest quality can bolster therapy efficacy, contributing to long-term emotional stability and better daily functioning. Tackling rest problems is not just a question of ease; it is an essential part of successful trauma recovery.
Future Directions in Treating Insomnia Secondary to PTSD
As research continues to evolve, innovative treatments for PTSD-related insomnia are gaining traction. Virtual reality exposure therapy and neuromodulation methods, like transcranial direct current stimulation (tDCS), have demonstrated considerable potential in tackling both disturbances during rest and post-traumatic stress disorder symptoms. In a recent study, participants receiving tDCS aimed at the ventromedial prefrontal cortex during virtual reality sessions reported a notable reduction in symptom severity related to post-traumatic stress. This approach not only accelerated psychological and physiological adjustments but also provided a less intrusive method for processing traumatic memories, making it more tolerable for patients who might otherwise drop out of traditional psychotherapy.
Moreover, the importance of understanding the lived experiences of patients from diverse backgrounds is emphasized in ongoing studies. This involves analyzing the effects of various forms of trauma, including severe accidents, physical or sexual violence, and experiences related to war, on rest and PTSD recovery. For instance, researchers have discovered that stress-related disturbances in rest significantly interfere with various processes in the body, emphasizing the necessity for therapies that can assist individuals in attaining more restorative slumber.
These emerging therapies offer a holistic approach to treatment, integrating the latest technological advancements with a deeper understanding of the complex relationship between trauma and sleep. As more studies are conducted, the path toward more effective and personalized treatment options for PTSD-related insomnia becomes clearer, offering hope for those seeking relief from their symptoms.
Conclusion
The intricate relationship between sleep and PTSD recovery underscores the vital role that restorative sleep plays in healing from trauma. Quality sleep not only facilitates memory consolidation but also regulates mood and enhances emotional resilience, which is essential for individuals navigating the challenges of PTSD. The prevalence of sleep disturbances among those with PTSD, including insomnia and nightmares, can create a cycle of heightened anxiety and emotional instability, making recovery more difficult.
Holistic and innovative approaches, such as cognitive behavioral therapy for insomnia and targeted memory reactivation, have shown promise in improving sleep quality and, consequently, PTSD symptoms. These non-pharmacological interventions, alongside pharmacological options, provide a comprehensive framework for addressing the multifaceted nature of sleep disturbances. By prioritizing sleep health and integrating these strategies into treatment plans, individuals can foster a more supportive environment for their healing journey.
As research continues to evolve, the exploration of new therapies, such as virtual reality exposure therapy and neuromodulation techniques, offers hope for more effective and personalized treatment options. Understanding the unique experiences of individuals from diverse backgrounds further enhances the potential for tailored interventions. Ultimately, addressing sleep disturbances is not just a matter of comfort; it is a crucial component of effective PTSD treatment and long-term emotional well-being.
By embracing the importance of sleep in the recovery process, individuals can take significant steps toward reclaiming their lives and improving their overall quality of life.




