PLEASE NOTE:
While the following article relates to your Google search, the services and methods at Goodwin Hypnosis may differ from those mentioned below. Since 2007, we have helped thousands of clients to overcome emotional and behavioral challenges when all else had failed. According to many of them (and their referring healthcare providers), our methods are faster than talk therapy, easier than willpower, and safer than medication. If you’re ready to resolve your issues, skip the article and visit the rest of our website, where you can learn about our unique approach, watch client testimonial videos, and discover how working with us one-on-one could be the solution you’ve been searching for.
We can help you with a variety of issues relating to emotional trauma. While we don't diagnose disorders like PTSD, we have helped hundreds of clients to overcome a wide range of traumatic experiences and their negative effects with methods that are more efficient and comfortable than CBT or EMDR. If you would like to learn more about working with us one-on-one to clear your trauma, click here.
Introduction
Post-Traumatic Stress Disorder (PTSD) often casts a shadow far beyond its well-known symptoms of anxiety, depression, and intrusive memories. One of the less discussed yet profoundly impactful consequences of PTSD is fatigue. The relentless state of heightened alertness and continuous stress depletes energy reserves, disrupting sleep and leaving individuals feeling perpetually exhausted.
This fatigue is not just a physical sensation but a deep, pervasive tiredness that affects daily functioning and quality of life.
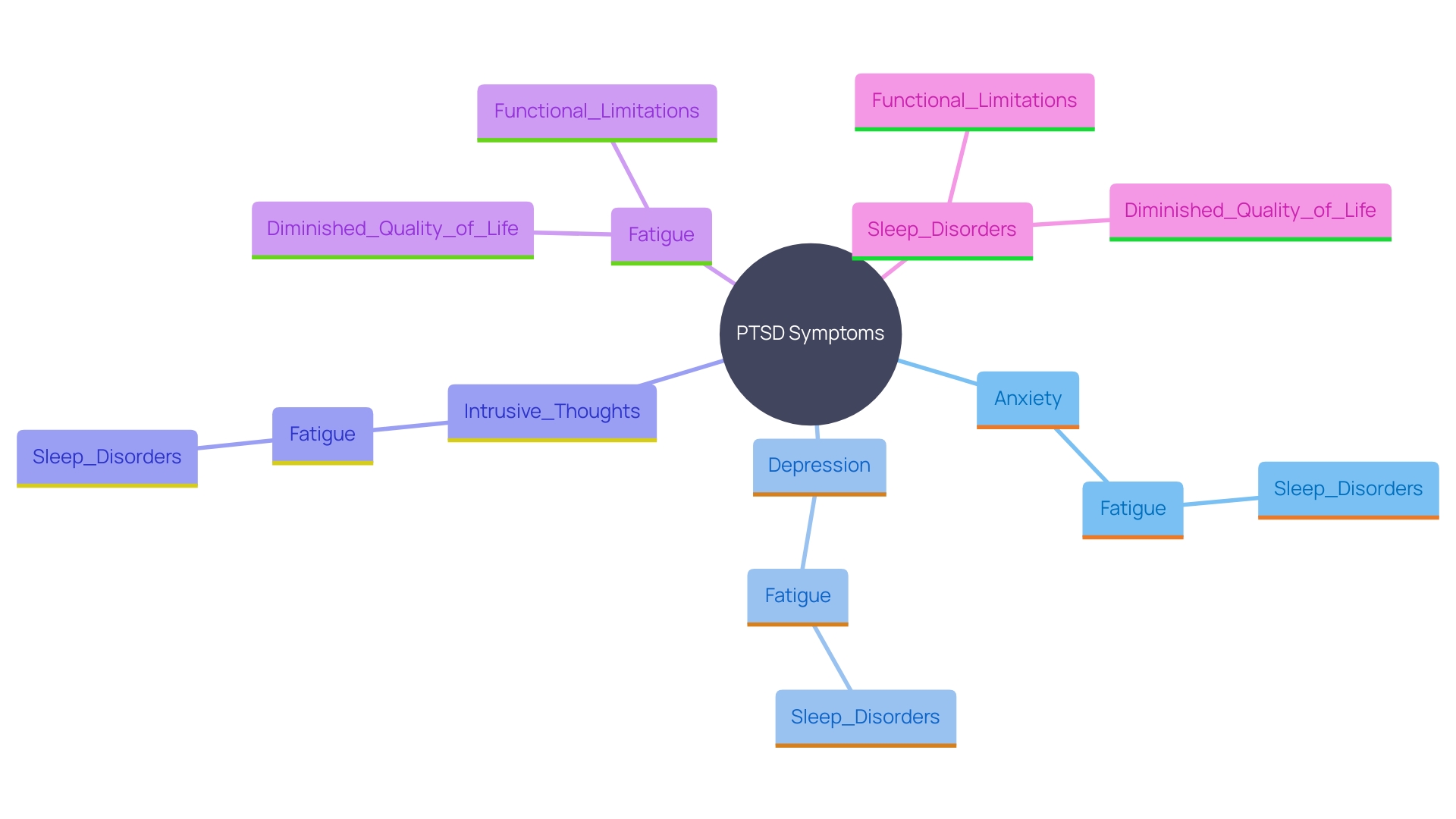
Research underscores a strong connection between PTSD-related fatigue and the emotional and psychological stress experienced by sufferers. Studies have shown that managing this fatigue can significantly improve patient outcomes and overall well-being. Moreover, the interplay between PTSD and anxiety disorders, which often lead to sleep disturbances, further exacerbates the sense of fatigue.
Understanding these interconnections is vital for developing effective interventions.
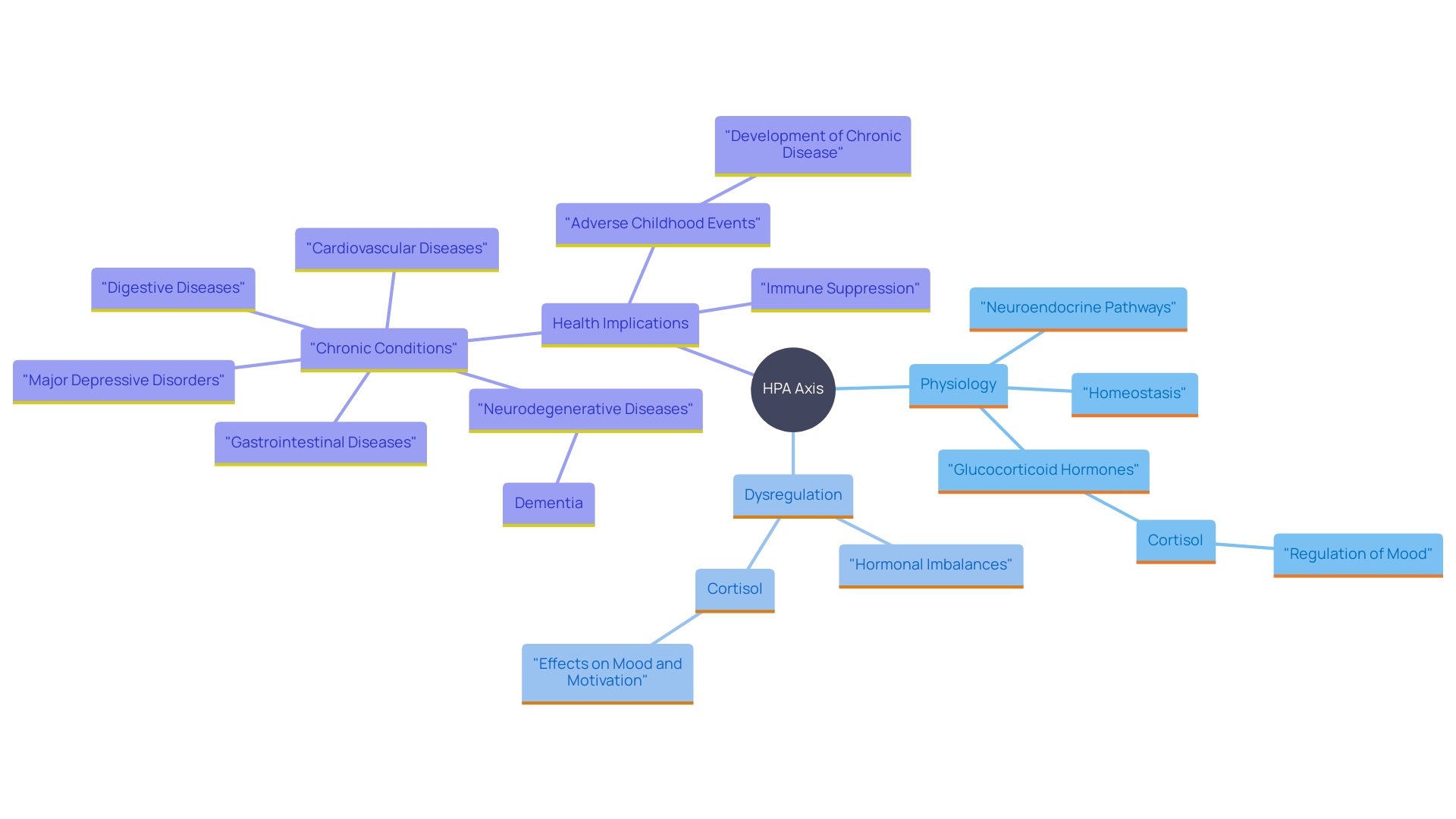
The neuroendocrine system, particularly the hypothalamic-pituitary-adrenal (HPA) axis, plays a crucial role in this dynamic. Dysregulation of this system in PTSD patients leads to hormonal imbalances, contributing to chronic fatigue and other health issues. Addressing PTSD-related fatigue thus requires a holistic approach that considers both mental and physical health.
Effective management strategies include a combination of cognitive-behavioral therapy, mindfulness practices, physical activities, balanced nutrition, and proper sleep hygiene. Real-life examples highlight the success of tailored, patient-centered approaches in alleviating fatigue and enhancing the quality of life for individuals with PTSD. Collaboration with healthcare professionals to develop personalized treatment plans is essential in navigating the complex landscape of PTSD and chronic fatigue.
The Psychological Impact of PTSD on Fatigue
Post-Traumatic Stress Disorder (PTSD) often manifests through a range of emotional and psychological symptoms such as heightened anxiety, depression, and intrusive thoughts. These symptoms can significantly contribute to feelings of tiredness. When people are consistently on high alert, their bodies stay in a constant state of tension, which results in fatigue. This psychological toll not only drains energy but also disrupts sleep patterns, intensifying the feeling of tiredness and leaving individuals feeling overwhelmed and depleted.
Research has shown that PTSD-related exhaustion is closely linked to the emotional and psychological stress experienced by sufferers. For instance, a study found that the identification of key themes and verbal descriptors can guide the development of techniques to handle tiredness, thereby improving patient outcomes and quality of life. This is essential as exhaustion forecasts functional limitations, diminished quality of life, and adverse health results such as disability and mortality.
Furthermore, anxiety disorders, which are common in individuals with post-traumatic stress issues, are linked to sleep disorders, further worsening fatigue. A China National Mental Health Survey indicated that anxiety, with a prevalence rate of 7.6%, is a complex emotional response that contributes to sleep disorders. The continuous interplay between anxiety and disrupted sleep in individuals with post-traumatic stress highlights the importance of addressing these interconnected issues.
Furthermore, studies involving individuals with post-traumatic stress disorder revealed significant differences in self-report measures compared to healthy controls, highlighting the severe impact of the condition on quality of life. Participants in such studies often report persistent exhaustion, a symptom that severely impacts their daily functioning and emotional well-being. These findings highlight the necessity for focused measures to reduce tiredness and enhance the overall quality of life for those experiencing post-traumatic stress.
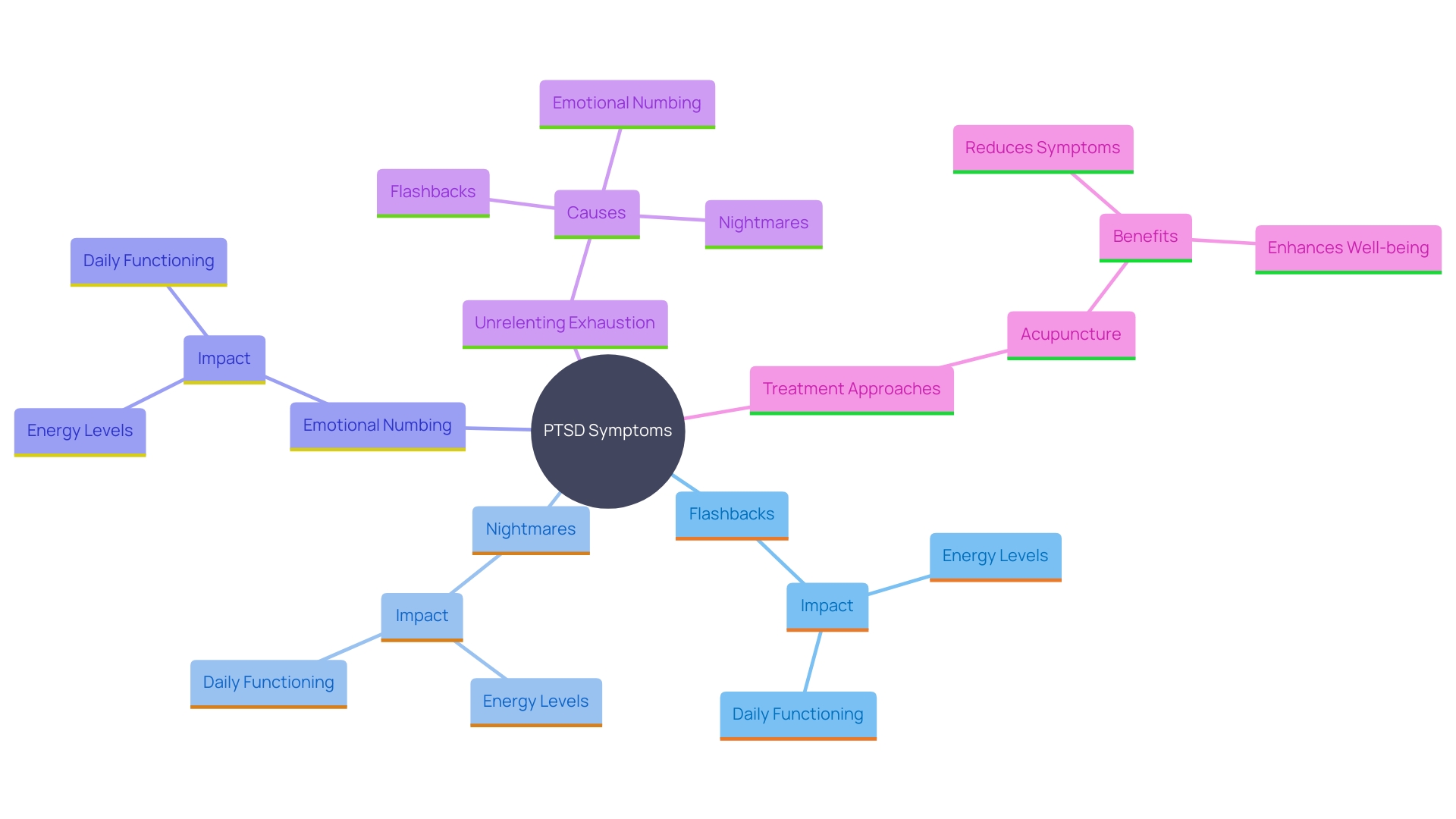
PTSD Symptoms and Their Relationship with Fatigue
The signs of post-traumatic stress disorder, including flashbacks, nightmares, and emotional numbing, can significantly reduce a person's energy levels. The mental effort required to manage these symptoms can be overwhelming. Numerous people with trauma-related stress disorder report difficulties in concentrating and sustaining attention, which additionally hinders everyday functioning and leads to ongoing tiredness. In a study, participants described their tiredness as unrelenting exhaustion, not relieved by rest, and interfering with usual activities. This underscores the necessity to recognize exhaustion as an essential element of post-traumatic stress disorder, stressing a caring method toward therapy. For instance, a clinical trial showed that acupuncture could effectively reduce symptoms of post-traumatic stress and improve overall well-being, suggesting that integrating such treatments might help alleviate fatigue and enhance quality of life.
The Neuroendocrine Connection: HPA Axis and Stress Response
The hypothalamic-pituitary-adrenal (HPA) axis is a critical component in the body's reaction to pressure. For individuals with PTSD, this system often becomes dysregulated, leading to hormonal imbalances, particularly with cortisol. Cortisol, the main hormone linked to pressure, plays a significant role in regulating mood, motivation, and fear. When the brain perceives danger, it triggers the release of cortisol to help the body respond. However, prolonged exposure to high cortisol levels due to ongoing pressure can lead to severe fatigue and burnout.
Research indicates that individuals with post-traumatic stress disorder frequently exhibit low glucocorticoid levels, which were initially thought to result from trauma exposure. Glucocorticoids, including cortisol, are produced by the adrenal glands and are vital for managing stress. As Carmen Sandi from the Swiss Federal Institute of Technology Lausanne (EPFL) explains, fluctuations in glucocorticoid levels among people can affect the chances of developing post-traumatic stress disorder. This understanding emphasizes why some individuals are more susceptible to post-traumatic stress than others, paving the way for more targeted treatments.
The neuroendocrine link between PTSD and exhaustion is further complicated by the body's reaction mechanisms to pressure. When the HPA axis is overstimulated, it can suppress the immune system, increase susceptibility to infections, and contribute to conditions like obesity and cardiovascular disease. This overactivation underscores the importance of viewing mental and physical health as interconnected. As clinical psychologist Rosalind S. Dorlen highlights, chronic stress can result in a variety of physical issues, underscoring the necessity for comprehensive methods in addressing PTSD-related exhaustion.
Managing PTSD and Chronic Fatigue Syndrome: Therapeutic Approaches
Effective management of PTSD-related exhaustion often requires a comprehensive approach. Cognitive-behavioral therapy (CBT) and mindfulness practices have demonstrated considerable advantages in managing both trauma-related symptoms and fatigue. For example, a combined mindfulness and yoga intervention in a U.S. Army study demonstrated improvements in mental health, showing that such practices are effective in managing high-stress occupations. Additionally, physical activities, balanced nutrition, and proper sleep hygiene are essential components of recovery.
Real-life examples further illustrate the effectiveness of these approaches. Megan, who manages her chronic health conditions and trauma-related stress, has found that pacing and prioritizing activities, along with a tailored flare-up plan, significantly improve her quality of life. Her ability to navigate daily pain without catastrophizing showcases the potential of well-rounded treatment plans. Another case emphasizes the significance of personalized care: Mike, a production packer with post-traumatic stress from a work injury, initially resorted to alcohol to manage. With appropriate intervention, including therapy and mindfulness practices, he managed to regain control over his life.
Working together with healthcare experts is essential in creating tailored treatment strategies that tackle the distinct overlap of post-traumatic stress disorder and chronic fatigue. As Dr. Rothbaum stated, “PTSD patients deserve the most effective treatments we can offer,” emphasizing the need for tailored and proactive care. This multifaceted approach fosters a pathway toward healing, ensuring that individuals like Megan and Mike can lead fulfilling lives despite their challenges.
Conclusion
The exploration of Post-Traumatic Stress Disorder (PTSD) reveals its profound impact on fatigue, a symptom often overshadowed by more visible emotional and psychological challenges. The relentless stress and hyper-vigilance associated with PTSD drain energy levels, disrupt sleep, and leave individuals feeling perpetually exhausted. Research highlights the intricate relationship between PTSD-related fatigue and the emotional burdens carried by sufferers, emphasizing that addressing this fatigue is crucial for improving overall well-being and quality of life.
The symptoms of PTSD, such as flashbacks and nightmares, not only deplete energy but also hinder daily functioning, leading to a cycle of unrelenting exhaustion. A compassionate acknowledgment of fatigue as a core component of PTSD is essential. Therapeutic approaches, including cognitive-behavioral therapy and mindfulness practices, have shown promise in alleviating both PTSD symptoms and associated fatigue, illustrating the importance of a holistic treatment strategy.
Furthermore, understanding the neuroendocrine connections, particularly the role of the HPA axis, sheds light on how chronic stress leads to hormonal imbalances that exacerbate fatigue. This interconnectedness of mental and physical health underscores the need for comprehensive management strategies that prioritize both aspects. Real-life examples demonstrate the effectiveness of personalized treatment plans that integrate various therapeutic modalities, emphasizing the importance of collaboration with healthcare professionals.
In summary, recognizing and addressing PTSD-related fatigue is vital for fostering recovery and enhancing the quality of life for those affected. By taking a multifaceted approach that encompasses psychological support, physical health, and tailored interventions, individuals can find pathways to healing and reclaim their lives from the shadows of PTSD.




