PLEASE NOTE:
While the following article relates to your Google search, the services and methods at Goodwin Hypnosis may differ from those mentioned below. Since 2007, we have helped thousands of clients to overcome emotional and behavioral challenges when all else had failed. According to many of them (and their referring healthcare providers), our methods are faster than talk therapy, easier than willpower, and safer than medication. If you’re ready to resolve your issues, skip the article and visit the rest of our website, where you can learn about our unique approach, watch client testimonial videos, and discover how working with us one-on-one could be the solution you’ve been searching for.
We can help you with a variety of issues relating to emotional trauma. While we don't diagnose disorders like PTSD, we have helped hundreds of clients to overcome a wide range of traumatic experiences and their negative effects with methods that are more efficient and comfortable than CBT or EMDR. If you would like to learn more about working with us one-on-one to clear your trauma, click here.
Introduction
Post-Traumatic Stress Disorder (PTSD) is a complex mental health condition that is often misunderstood and surrounded by numerous myths. These misconceptions not only stigmatize those affected but also hinder their path to recovery by perpetuating false beliefs. From questioning the legitimacy of PTSD to assuming it only affects certain groups or manifests immediately, these myths can prevent individuals from seeking the help they need.
Understanding the realities of PTSD is essential to providing the empathy and support necessary for healing. This article aims to debunk common myths about PTSD, shedding light on the true nature of the condition and the varied experiences of those who live with it. By dispelling these myths, a more compassionate and informed perspective can be fostered, ultimately aiding in the journey toward recovery and well-being for those affected by PTSD.
Myth 1: PTSD is Not a Real Condition
Post-Traumatic Stress Disorder is a recognized mental health condition that can arise following the experience or observation of a traumatic event. It is classified in the Diagnostic and Statistical Manual of Mental Disorders (DSM) and is supported by extensive research. This myth undermines the struggles of those who live with post-traumatic stress disorder, dismissing their pain and experiences as invalid. Comprehending post-traumatic stress disorder as a genuine condition is essential to nurturing compassion and assistance for individuals impacted.
Research has found that women are twice as vulnerable to post-traumatic stress disorder compared to men, which is alarming given the high prevalence of experiences that trigger this condition in the world today. Studies have estimated that almost all women in the United States will experience at least one major traumatic event over the course of their lives. 'The impact of post-traumatic stress disorder extends beyond mental health, with growing evidence showing its cardiovascular and neurocognitive effects, such as cardiovascular disease and dementia, which are major causes of female mortality.'.
At the core of post-traumatic stress disorder is a memory that cannot be controlled, often intruding on everyday activities and surfacing as night terrors or flashbacks. Decades of research on military veterans and sexual assault survivors have shown that traumatic memories function differently from other memories. For example, a team of scientists at Yale University and the Icahn School of Medicine at Mount Sinai discovered tangible proof of these variations by performing brain scans on individuals with post-traumatic stress disorder while they listened to recorded accounts of their own memories.
Real-life stories further illustrate the profound impact of post-traumatic stress disorder. Julia, a military veteran, experienced intense psychological trauma after witnessing a Harrier jet burst into flames during her deployment. Likewise, Marty and Candy Larsen's daughter displayed signs of trauma, including episodes of intense fear and disconnection from reality.
Given these facts, it's clear that post-traumatic stress disorder requires serious clinical and psychological interventions. The condition is not a reflection of personal weakness but a legitimate mental health issue that necessitates understanding and assistance. As one expert noted, treatment for post-traumatic stress disorder is effective, and seeking help is a sign of strength. Through empathy and proper support, we can help those impacted by post-traumatic stress to heal and lead fulfilling lives.
Myth 2: PTSD Only Affects Military Veterans
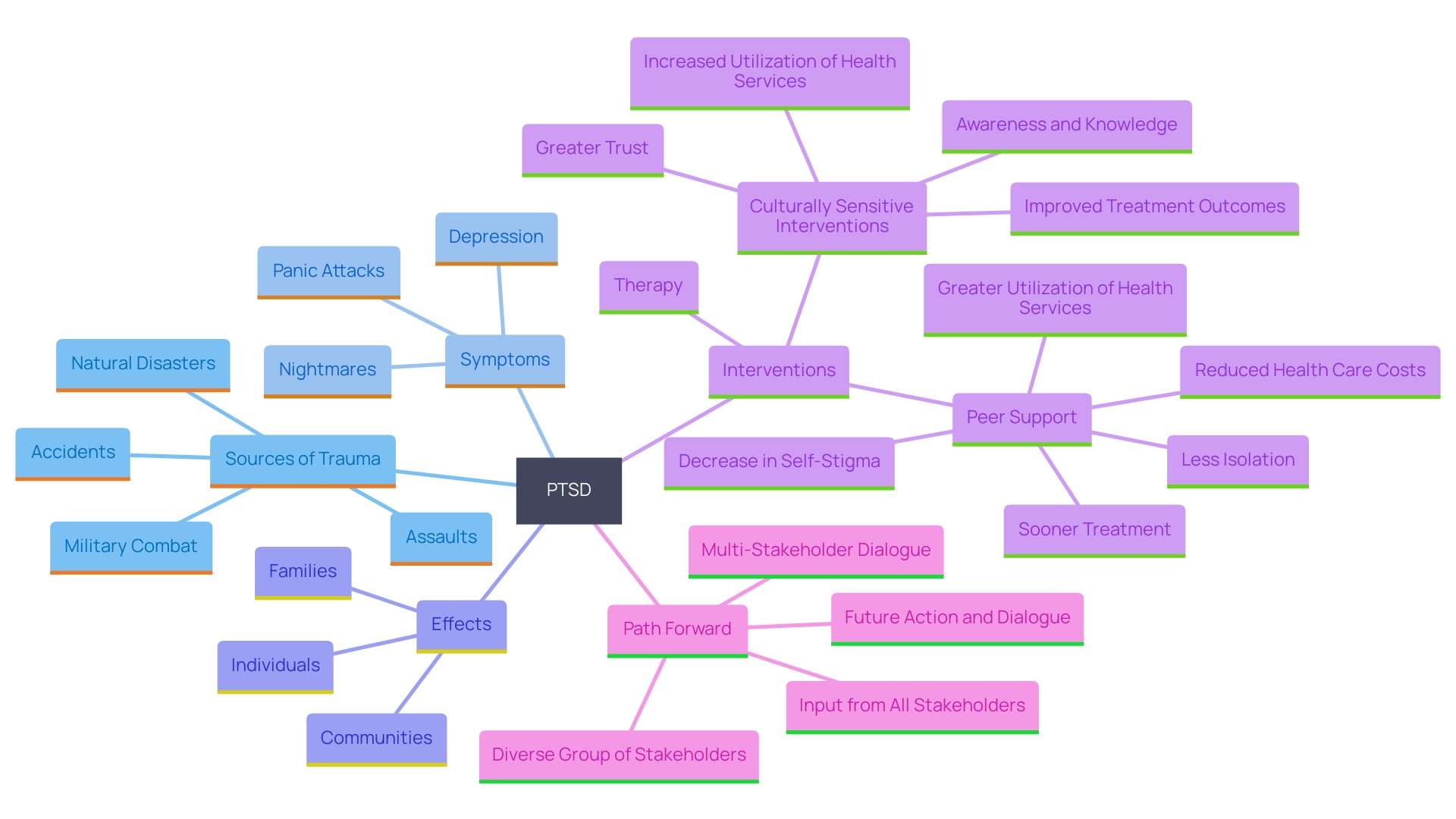
While it is true that many military veterans experience post-traumatic stress due to combat exposure, this condition can affect anyone who has undergone distressing events. This includes survivors of accidents, natural disasters, assaults, and other distressing events. An investigation by The New York Times found that many of the troops sent to bombard the Islamic State in 2016 and 2017 returned to the United States plagued by nightmares, panic attacks, depression, and, in a few cases, hallucinations. Once-reliable Marines turned unpredictable and strange, with some even becoming homeless or attempting suicide. Research shows a clear association between military sexual trauma and mental health conditions, including post-traumatic stress disorder, depression, and suicidal ideation.
Furthermore, Dr. Sofia Matta from Harvard-affiliated Massachusetts General Hospital highlights that post-traumatic stress disorder doesn't only impact the individual experiencing it but also their families and communities. It's important to recognize that post-traumatic stress disorder can impact individuals from all walks of life. Research has indicated that therapy can assist in alleviating symptoms of post-traumatic stress and depression, which may occasionally appear years after the distressing incident. Culturally sensitive interventions and peer assistance can play crucial roles in addressing the unique needs of those affected, fostering greater trust and improving overall treatment outcomes. By acknowledging that post-traumatic stress disorder can affect people from all backgrounds, we can foster a more inclusive conversation that supports diverse experiences of trauma.
Myth 3: PTSD Occurs Immediately After a Traumatic Event
It is frequently misinterpreted that PTSD indicators appear immediately following a traumatic event. However, signs can emerge months or even years later. This delayed onset can be triggered by reminders of the distressing event or significant life changes. For instance, some veterans may not encounter symptoms of post-traumatic stress until they retire, as the organization of their professional life earlier assisted them in coping with their difficulties. Understanding this delayed timeline is crucial, as it underscores the importance of recognizing and addressing the ongoing impact of trauma.
Post-traumatic stress disorder can lead to severe anxiety, depression, and substance abuse, significantly affecting one's quality of life. Research has indicated that women are twice as likely to develop post-traumatic stress disorder compared to men, with almost all women in the US experiencing a significant traumatic event in their lifetime. 'This high prevalence, combined with the potential for issues to arise later in life, makes awareness and early intervention essential.'.
Reactions to past distressing events can be grouped into several types: reliving the incident through flashbacks and nightmares, steering clear of reminders of the occurrence, and undergoing unfavorable shifts in thought and emotion. Identifying these signs, even if they emerge long after the initial injury, is crucial for obtaining suitable care and assistance. Clinical and psychological interventions, along with social support, can significantly improve outcomes for those affected by post-traumatic stress disorder.
Myth 4: Everyone Who Experiences Trauma Will Develop PTSD
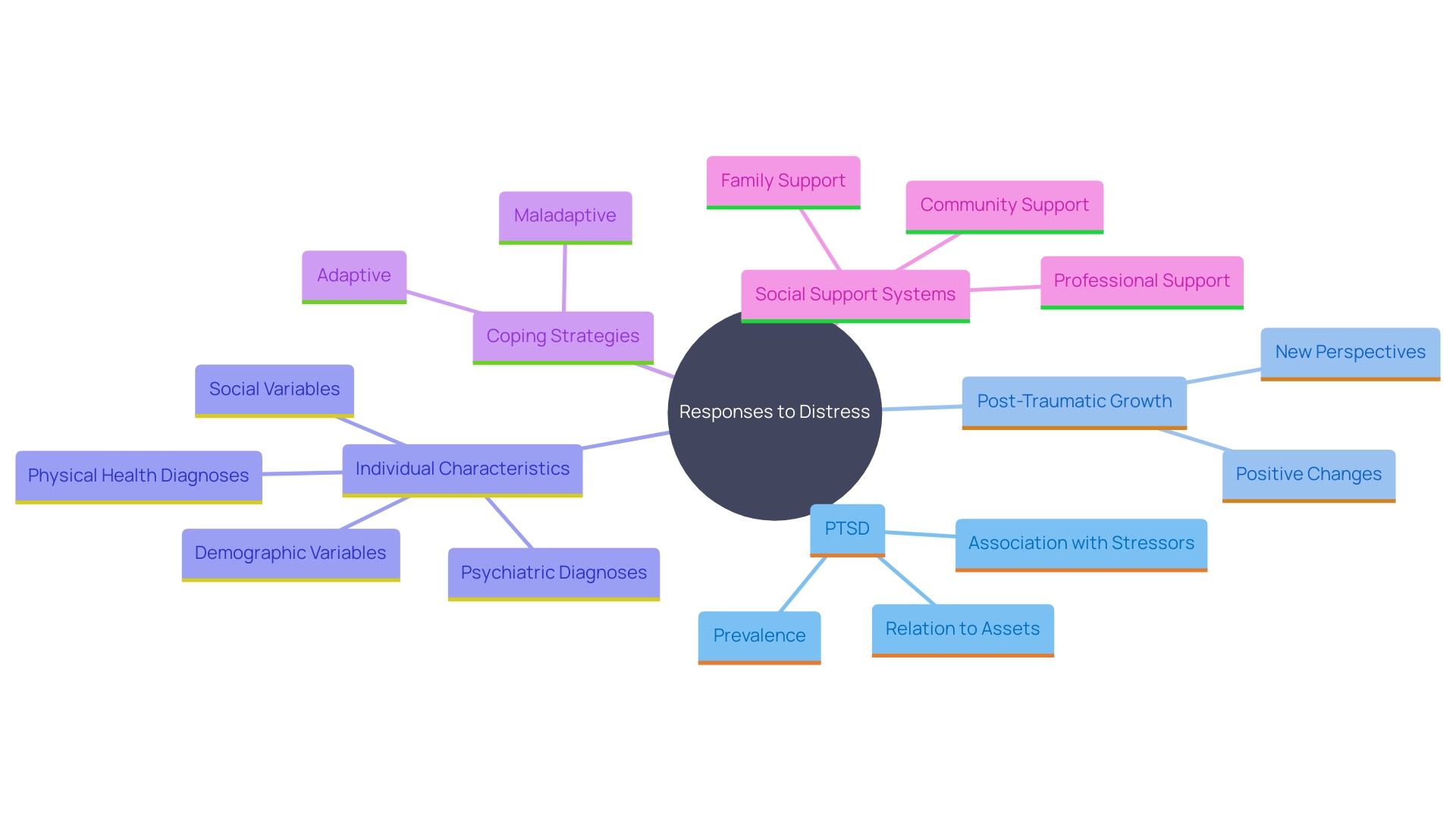
Not everyone who undergoes distress will develop PTSD, a fact that underscores the diverse ways individuals respond to traumatic events. According to researchers Richard Tedeschi, PhD, and Lawrence Calhoun, PhD, experiencing tragedy or crisis can sometimes lead to post-traumatic growth, which involves positive psychological changes in self-perception, relationships, and life philosophy. This phenomenon occurs in approximately 30-90% of individuals who have experienced distress, highlighting the potential for resilience and recovery.
Personal reactions to distress are shaped by multiple elements, such as individual background, coping strategies, and assistance networks. For example, the emerging field of neuroresilience explores why people respond differently to stress and trauma, suggesting that physiological mechanisms play a significant role in these varied responses.
Furthermore, resilience is not only influenced by personal characteristics but also by social factors like assistance networks and available resources. A study from Tulane University emphasizes that support systems and resources significantly contribute to resilience, especially in the context of long-term recovery from large-scale disasters.
Grasping the intricacy of emotional reactions is essential. 'While some individuals may develop post-traumatic stress disorder, characterized by symptoms like intrusive memories, avoidance, and negative changes in cognition and mood, others may find strength and growth in their experiences.'. As a clinical psychologist working with first responders, I have witnessed individuals realize their inner strength and develop greater empathy, leading to enhanced connectedness with others.
Acknowledging this variability is essential for a comprehensive understanding of trauma and its effects, paving the way for effective support and intervention strategies tailored to individual needs.
Myth 5: PTSD Always Leads to Violent Behavior
A common misconception about post-traumatic stress disorder is that it makes individuals prone to violence. In reality, individuals with post-traumatic stress disorder are more prone to encountering issues such as anxiety, depression, and emotional turmoil instead of aggression. This stereotype perpetuates stigma and prevents those affected from seeking the help they need. Studies have indicated that trauma-related issues frequently start within three months of a distressing occurrence, though they may occasionally surface years afterward. For a diagnosis of post-traumatic stress disorder, these signs must last for over a month and frequently occur alongside depression, anxiety, or substance use.
Furthermore, post-traumatic stress disorder can develop in both adults and children, and the frequency differs depending on various risk factors, including previous trauma and the amount of social support present. The biological 'fight-or-flight' response, while crucial during a crisis, can leave lasting symptoms that affect one's daily life. Recent studies have even connected post-traumatic stress disorder to other health issues, such as cardiovascular disease and neurocognitive impacts, highlighting the extensive effects of the condition.
Experts emphasize the importance of addressing these misconceptions to reduce stigma and encourage individuals to seek appropriate treatment. As post-traumatic stress disorder cannot be cured, it can be managed through various therapies, including cognitive processing therapy and group therapy. Addressing and understanding these myths is vital for supporting those on their journey to healing.
Myth 6: People with PTSD Cannot Function Normally
Contrary to the widespread myth, individuals with post-traumatic stress disorder can and do lead fulfilling lives. While post-traumatic stress disorder presents challenges, many individuals learn to manage their symptoms effectively through appropriate support and treatment. This encompasses therapy, which has been shown to be effective even for those who have undergone numerous distressing experiences. For example, a review of over 130 clinical trials discovered that adults with post-traumatic stress disorder resulting from multiple traumas gained just as much from therapy as those with single-event post-traumatic stress disorder.
Symptoms of PTSD, which include re-experiencing traumatic events, avoidance behaviors, and cognitive and mood disruptions, can be daunting. However, with the right interventions, many individuals successfully navigate their daily lives, maintaining work, relationships, and other activities. Studies have indicated that elements such as social encouragement can greatly enhance resilience, allowing those impacted to regain control over their lives.
The story of Yelena, a young girl in a war-torn refugee camp, underscores the importance of timely intervention and support. Despite her traumatic experiences, with the help of dedicated professionals, she began to find a path to recovery. This highlights that with the right resources and care, the stereotype of dysfunction associated with post-traumatic stress disorder can be effectively challenged.
In essence, post-traumatic stress disorder is a complex but manageable condition. With ongoing research and evolving treatment methods, many individuals continue to defy the myths, leading lives that are not only normal but also deeply rewarding.

Myth 7: PTSD Will Just Go Away Over Time
It is a widespread misunderstanding that post-traumatic stress disorder will naturally fade over time without any form of intervention. However, while some indicators might diminish, untreated post-traumatic stress can lead to enduring and serious difficulties that greatly affect an individual's everyday existence and overall health. Prompt assistance and successful care are essential for individuals experiencing post-traumatic stress disorder. For instance, Mike, a 49-year-old production packer, sustained severe third-degree burns on his hand during a work accident. His vivid recollections of the incident, combined with the persistent odor of charred flesh, illustrate how intrusive and distressing the effects of trauma can be. These symptoms include flashbacks, avoidance behaviors, negative changes in thoughts and mood, and heightened arousal.
Research has demonstrated that trauma-focused therapies, such as cognitive processing therapy and prolonged exposure therapy, are especially effective for addressing post-traumatic stress disorder. These therapies help individuals reframe their traumatic experiences and reduce the negative impact on their mental health. Additionally, new studies have highlighted the importance of peer support, which can significantly decrease feelings of isolation and encourage individuals to seek treatment.
Moreover, tackling the effects of trauma early can avert the emergence of persistent problems such as sleeplessness and ongoing discomfort, which are frequently linked to the condition. For example, the PCL-5 self-report measure, which quantifies trauma-related symptoms, can help clinicians assess the severity of the condition and tailor appropriate interventions.
In summary, while some may believe that this disorder will fade with time, evidence strongly supports the need for early and targeted interventions to facilitate healing and improve quality of life for those affected by this condition.
Myth 8: PTSD Symptoms Are Always the Same
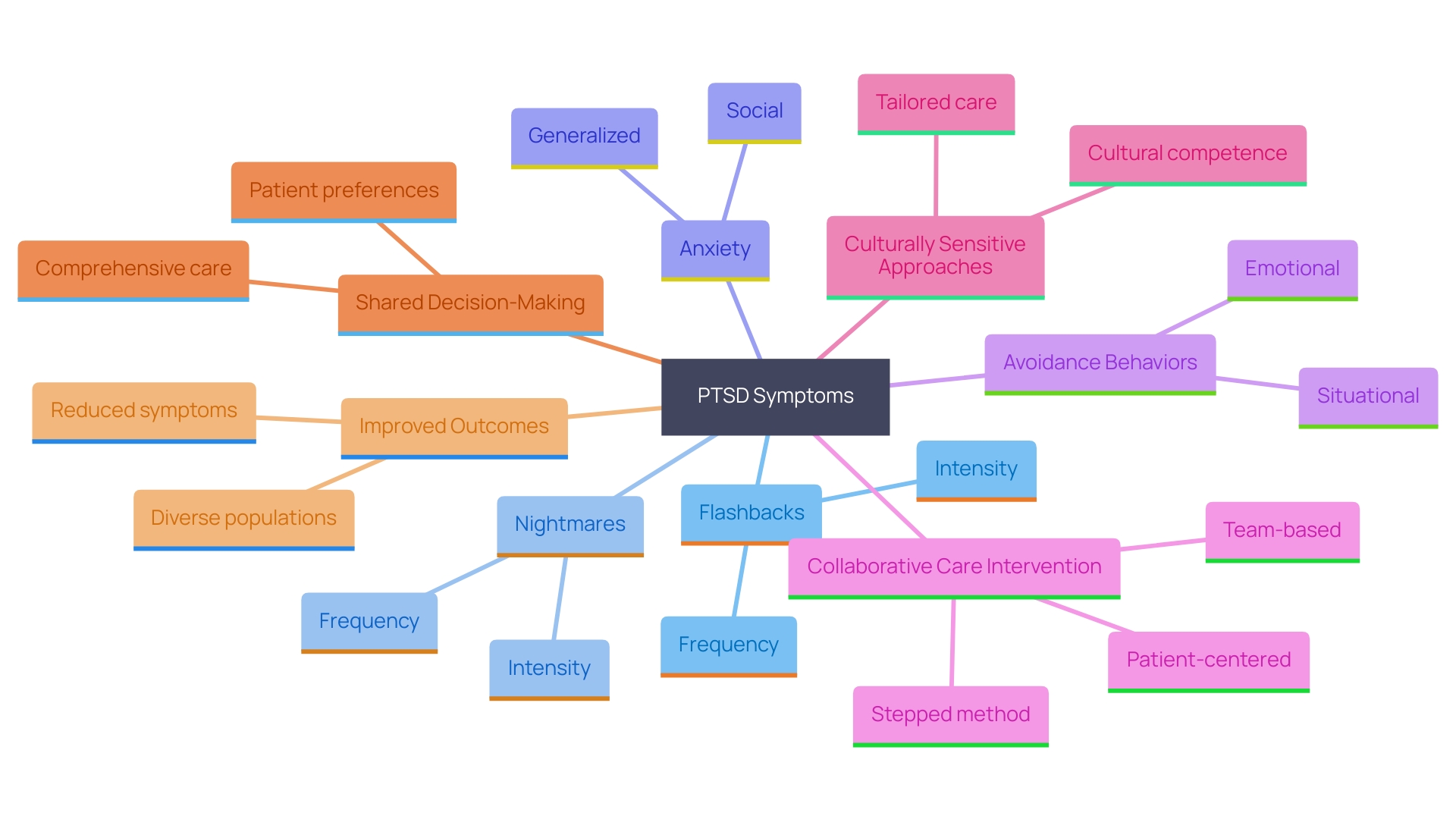
Symptoms of post-traumatic stress disorder can vary widely among individuals and even within the same person over time. Frequent signs include flashbacks, nightmares, anxiety, and avoidance behaviors, but the intensity and expression of these signs can differ significantly. Acknowledging the variety of trauma-related issues is essential for creating effective therapeutic approaches and promoting awareness among individuals who may not identify their own situations.
A recent study funded by the National Institute of Mental Health highlights the importance of tailored treatment approaches. This study found that a collaborative care intervention, which involves a team-based, patient-centered approach, significantly reduced PTSD symptoms among patients from racial and ethnic minority backgrounds. This approach is flexible and adjusts based on the patient's condition and response to treatment, showing promising results in real-world settings.
The study's success is attributed to its comprehensive care model, which focuses on the patient's needs and preferences and emphasizes shared decision-making. This method has shown to be effective in addressing the unique mental health needs and disparities experienced by different racial and ethnic groups. This real-world impact is now informing trauma care guidelines in the United States, with trauma centers implementing a screening and referral process for patients at high risk for mental disorders after injury.
Furthermore, culturally sensitive interventions, including peer support, have been found to increase the utilization of health services and foster greater trust between patients and clinicians. This leads to improved treatment outcomes and highlights the importance of recognizing and addressing the diverse symptoms and needs of those living with PTSD.
Conclusion
Understanding the complexities of Post-Traumatic Stress Disorder (PTSD) is essential in dispelling the myths that often surround it. The recognition that PTSD is a legitimate mental health condition, affecting individuals from all walks of life, is vital in fostering empathy and support. Myths such as the notion that PTSD only affects military veterans or that symptoms manifest immediately after trauma overlook the diverse experiences and realities faced by those living with this condition.
Moreover, acknowledging that not everyone who experiences trauma will develop PTSD, and that the symptoms can vary widely among individuals, reinforces the importance of a tailored approach to treatment. Early intervention is crucial, as untreated PTSD can lead to long-lasting challenges. The misconception that PTSD will simply fade over time can deter individuals from seeking the help they need, highlighting the importance of education and awareness.
Ultimately, addressing these myths is vital for creating a supportive environment where individuals feel empowered to seek help and pursue healing. By fostering understanding and compassion, society can contribute to the recovery journey of those affected by PTSD, ensuring they receive the care and support necessary to lead fulfilling lives.




