PLEASE NOTE:
While the following article relates to your Google search, the services and methods at Goodwin Hypnosis may differ from those mentioned below. Since 2007, we have helped thousands of clients to overcome emotional and behavioral challenges when all else had failed. According to many of them (and their referring healthcare providers), our methods are faster than talk therapy, easier than willpower, and safer than medication. If you’re ready to resolve your issues, skip the article and visit the rest of our website, where you can learn about our unique approach, watch client testimonial videos, and discover how working with us one-on-one could be the solution you’ve been searching for.
We can help you with a variety of issues relating to emotional trauma. While we don't diagnose disorders like PTSD, we have helped hundreds of clients to overcome a wide range of traumatic experiences and their negative effects with methods that are more efficient and comfortable than CBT or EMDR. If you would like to learn more about working with us one-on-one to clear your trauma, click here.
Introduction
Sleep disturbances are a common yet debilitating consequence for those living with PTSD, casting a long shadow over their daily lives and overall well-being. Difficulty falling asleep, frequent awakenings, and distressing nightmares are just a few of the sleep issues that plague individuals, often perpetuating a relentless cycle of fear and anxiety. Studies have underscored the stark contrast in sleep quality, latency, and efficiency between PTSD sufferers and those without the disorder.
Innovative treatments like lucid dreaming workshops and targeted memory reactivation during sleep are emerging as promising solutions to transform these distressing nighttime experiences. Understanding the intricate interplay between trauma, anxiety, and sleep disturbances is crucial for developing effective, comprehensive treatment plans that not only improve sleep but also enhance the quality of life for those affected by PTSD.
Common Sleep Disturbances in PTSD
People with post-traumatic stress disorder often experience different rest issues that greatly affect their overall health. Common issues include difficulty falling into slumber, frequent awakenings, and distressing nightmares often linked to their traumatic experiences, thus perpetuating a cycle of fear and anxiety that hinders restorative rest. Furthermore, a 2022 study emphasized that PTSD patients report significantly poorer rest quality, longer latency to rest, and reduced rest efficiency compared to healthy controls. They also undergo more awakenings and a longer REM rest latency. A creative method to reduce distressing dreams involves lucid dreaming workshops, where participants learn to induce and utilize lucid dreams to change their troubling dreams and integrate trauma. This method has shown promise in enhancing rest quality and reducing nightmare frequency. Furthermore, studies have found a significant occurrence of breathing interruptions during rest and rhythmic limb motions in individuals with trauma-related disorders, which further leads to disturbed resting patterns. Tackling these nightly issues necessitates thorough treatment strategies, incorporating methods such as CBT for insomnia, which have shown considerable enhancements in rest-related and emotional results.
Causes of Sleep Problems in PTSD
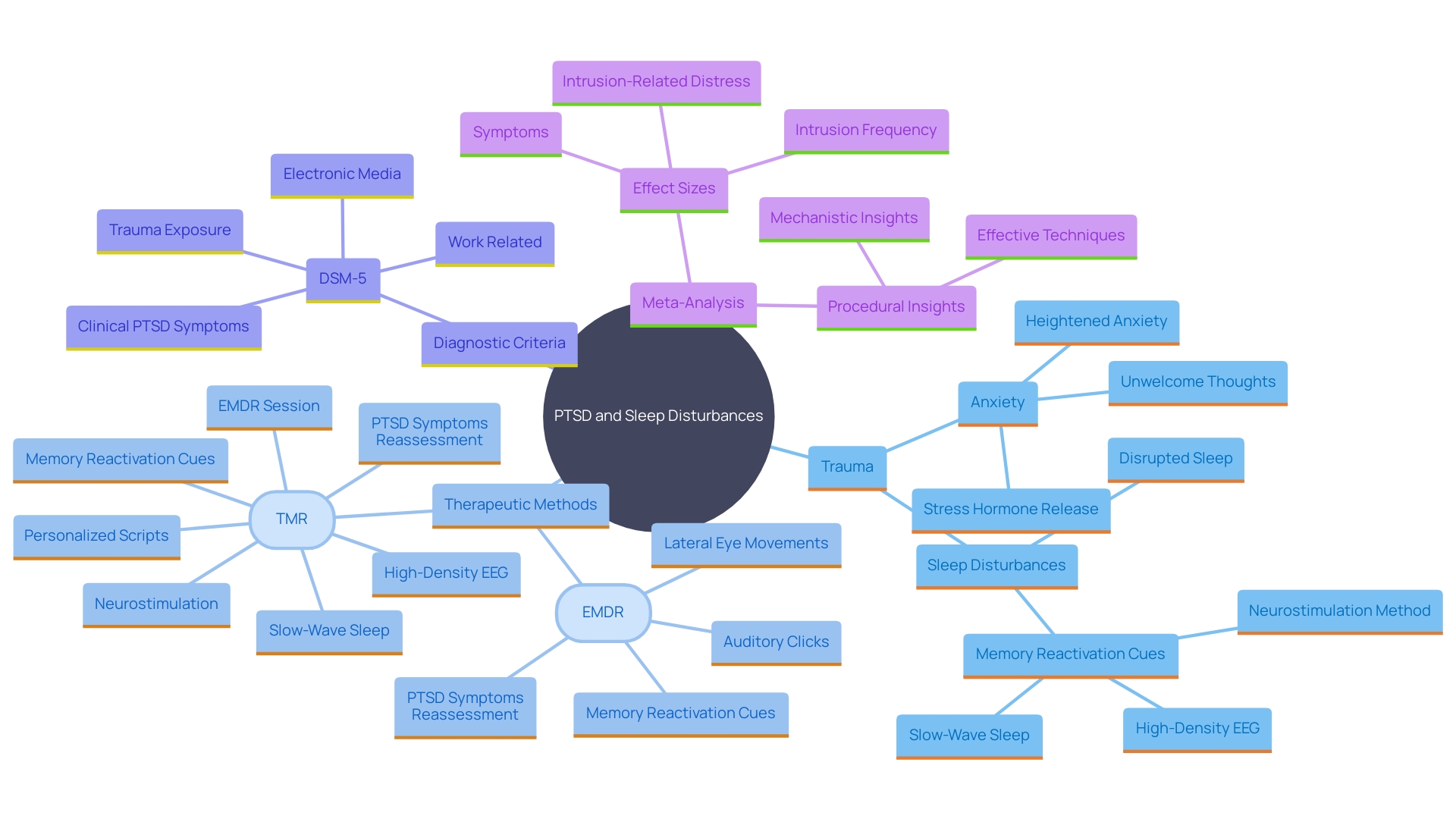
Sleep disturbances linked to post-traumatic stress can be traced to several interrelated factors. Trauma often results in heightened anxiety and hyperarousal, making it challenging for the brain to relax into a restful state. This is compounded by the brain's increased release of stress hormones following trauma, which disrupts normal rest patterns. People with post-traumatic stress disorder often encounter unwelcome thoughts or recollections at night, hindering them from attaining rejuvenating rest. The emotional and mental burden of post-traumatic stress disorder generates a harmful cycle in which rest disruptions worsen the disorder's symptoms, making recovery more challenging.
One groundbreaking approach to mitigating these rest issues is through targeted memory reactivation (TMR) during slumber. In a recent study, participants with post-traumatic stress disorder underwent a session of eye movement desensitization and reprocessing (EMDR) before resting. During the night, memory reactivation cues were introduced in sync with specific phases of slow-wave slumber, a stage crucial for memory consolidation. Monitoring brain activity with high-density electroencephalography (EEG), researchers found significant improvements in trauma-related symptoms the following morning and one week later.
Furthermore, the occurrence of sleep disorders and periodic limb movements in individuals with post-traumatic stress symptoms can lead to frequent awakenings and diminished rest quality. Studies have shown that sleep-related issues, including insomnia, are prevalent among those with chronic conditions and anxiety. For instance, a survey of around 1,000 Vietnamese people diagnosed with COVID-19 found that three-in-four reported insomnia, particularly those with pre-existing conditions.
Comprehending the complex connection among trauma, anxiety, and rest issues is essential. As one expert noted, 'Sleep issues can be a sign of an impending condition such as bipolar disorder. Many medical and mental health conditions can worsen due to sleep-related problems.' Tackling issues related to rest through creative therapies such as TMR and EMDR provides optimism for enhancing the quality of life for those experiencing trauma-related challenges.
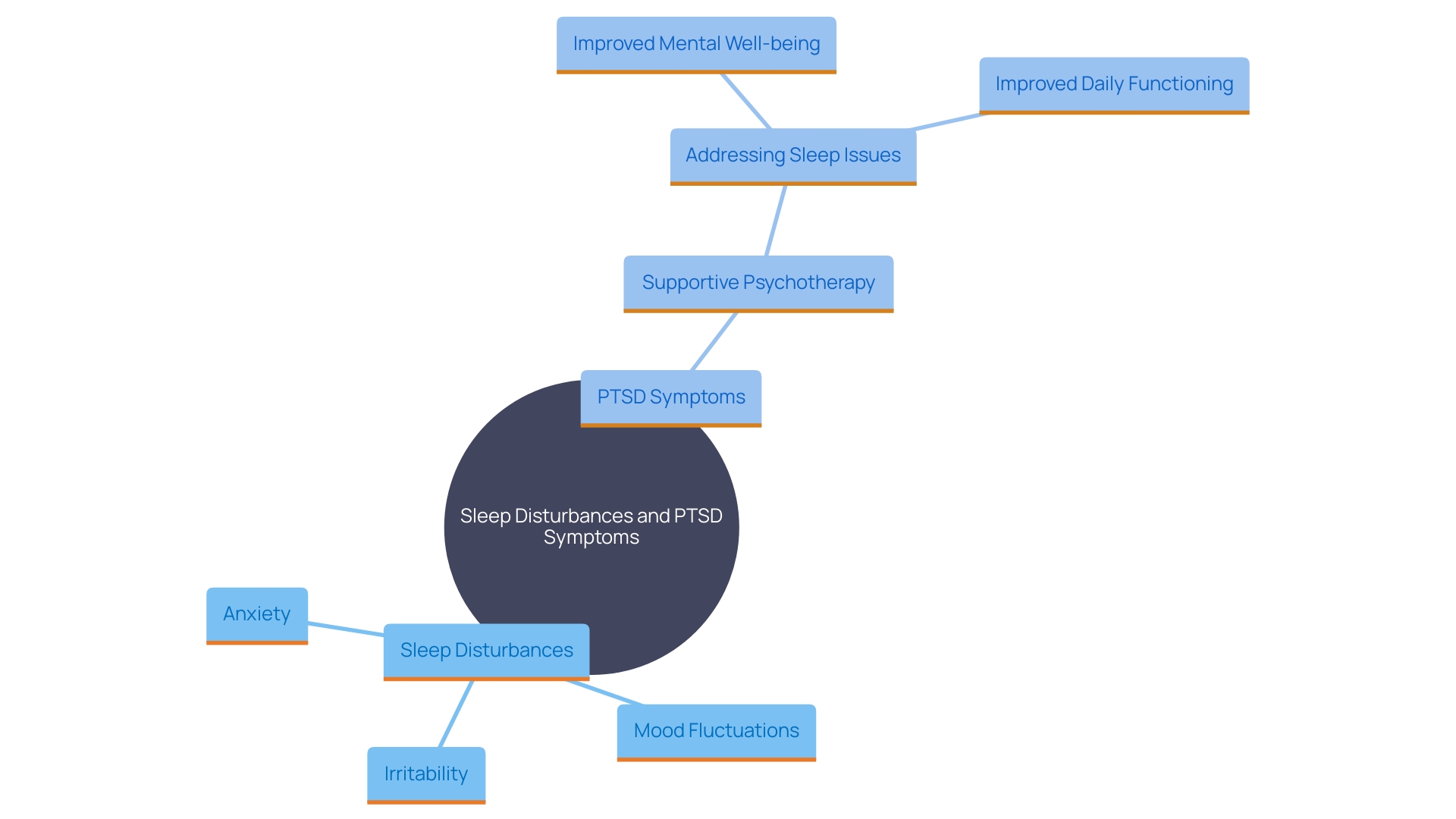
Impact of Sleep Problems on PTSD Symptoms
Sleep disturbances have a profound impact on the severity of PTSD symptoms. Inadequate rest can result in heightened irritability, mood fluctuations, and trouble focusing, which can obstruct everyday functioning. The absence of restorative rest can also amplify feelings of anxiety and depression, making it harder for individuals to cope with the aftermath of their trauma. Furthermore, the experience of bad dreams can trigger flashbacks or heightened emotional responses, perpetuating a cycle of fear and distress. Studies indicate that troubling dreams and distressing experiences during rest can disrupt proper slumber, resulting in subsequent issues with emotional control and general mental and physical well-being. Frequent nightmares might affect up to 70% of individuals with post-traumatic stress disorder, increasing anxiety and distress and impairing daytime functioning. Successful handling of rest problems is essential for people aiming to ease their trauma-related symptoms and enhance their overall well-being. Interventions like supportive psychotherapy have demonstrated a notable enhancement in results, lowering anxiety levels and enhancing rest quality in individuals. Tackling insomnia symptoms can result in improved daytime performance and overall mental well-being, emphasizing the significance of thorough care for individuals experiencing trauma-related stress.
Treatment Approaches for PTSD-Related Sleep Problems
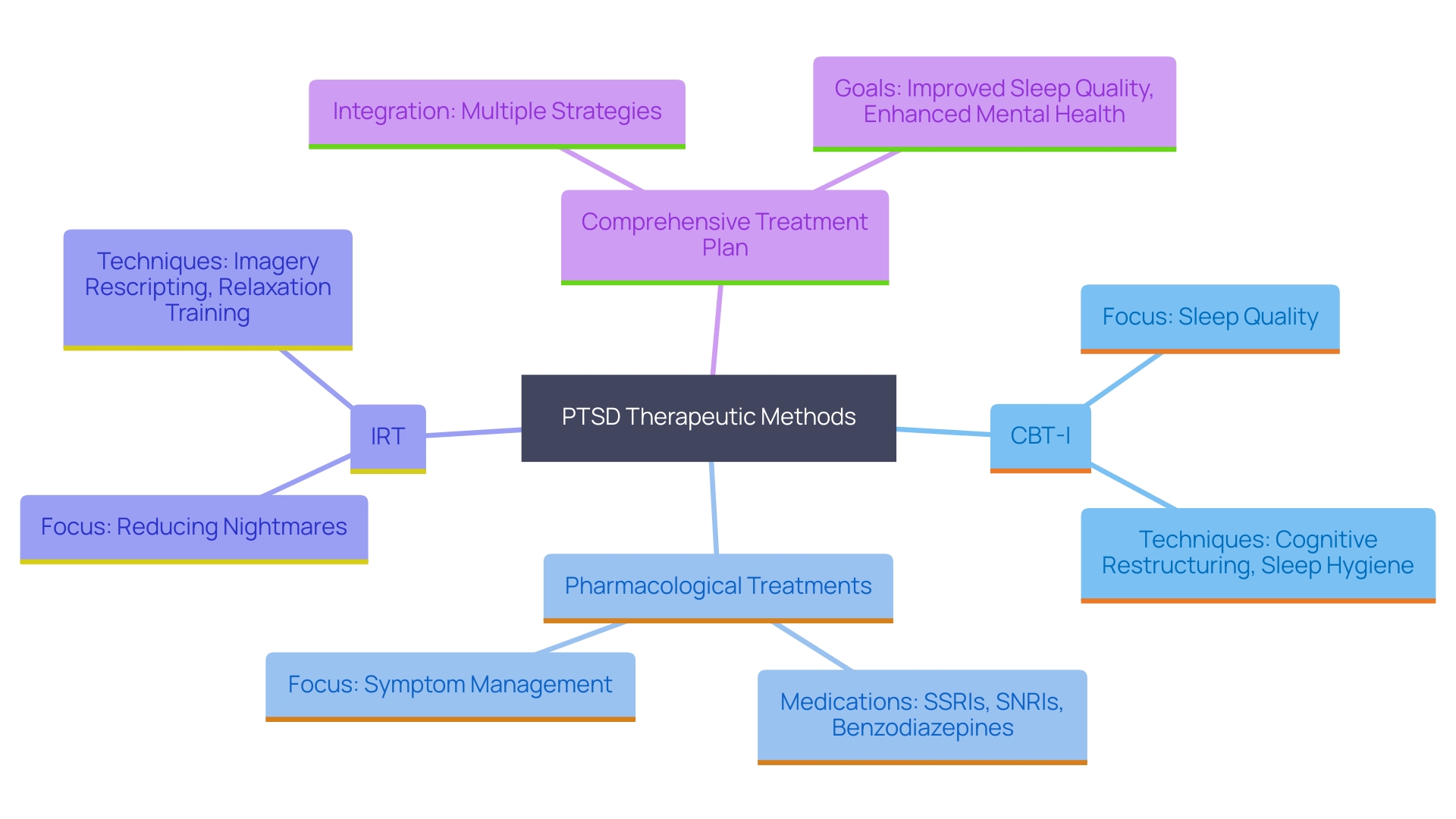
Tackling disturbances in individuals with PTSD requires a multifaceted approach that combines various therapeutic methods. Cognitive Behavioral Therapy for Insomnia (CBT-I), acknowledged for its effectiveness, concentrates on changing unproductive thoughts and actions related to rest. This method assists individuals in cultivating healthier rest habits and reducing anxiety associated with slumber. As noted by Yuki Furukawa, a leading researcher, CBT-I encompasses a broad range of strategies, and in-person interaction with a therapist has been found to be particularly beneficial.
Pharmacological treatments, such as certain antidepressants or sleep aids, may also be prescribed to manage symptoms effectively. Studies indicate that 19% of interventions for post-traumatic stress disorder involve pharmacologic treatments, which can be essential for some patients. However, medications often come with significant adverse effects, highlighting the need for alternative therapies.
Imagery Rehearsal Therapy (IRT) is another valuable approach, specifically targeting nightmares. This therapy assists individuals in reframing their traumatic dreams, providing significant relief. Case studies have shown that therapies like CBT-I and IRT can be effectively conducted via telehealth, providing greater accessibility for patients.
Integrated treatment strategies that combine various methods, including CBT-I, pharmacological treatments, and IRT, often yield the best outcomes. Studies carried out at Northwestern University showed that merging these methods can effectively tackle both trauma-related issues and related rest problems. The research, which included individuals from a VA Medical Center, emphasized that those who underwent a blend of treatments saw notable enhancements in rest quality and a decrease in trauma-related symptoms.
In conclusion, a comprehensive and personalized treatment plan that integrates multiple therapeutic options offers the most effective solution for managing disturbances in individuals with PTSD. This approach not only improves sleep quality but also enhances overall mental health and well-being.
Conclusion
Sleep disturbances are a significant challenge for individuals living with PTSD, often exacerbating the symptoms of anxiety and depression. The interplay between trauma and sleep issues creates a vicious cycle that can hinder recovery and diminish quality of life. It is essential to recognize the various sleep problems associated with PTSD, such as difficulty falling asleep, frequent awakenings, and distressing nightmares.
These disturbances not only affect sleep quality but also contribute to increased irritability and emotional turmoil.
Innovative treatment approaches, including Cognitive Behavioral Therapy for Insomnia (CBT-I), Imagery Rehearsal Therapy (IRT), and targeted memory reactivation (TMR), have emerged as promising solutions. These therapies aim to address the root causes of sleep disturbances, helping individuals develop healthier sleep habits and reshape their nighttime experiences. Importantly, combining these methods often yields the most effective results, leading to significant improvements in both sleep quality and PTSD symptoms.
Ultimately, understanding and addressing sleep disturbances is crucial for those dealing with PTSD. A comprehensive treatment plan that incorporates various therapeutic options not only aids in restoring restful sleep but also fosters emotional healing and resilience. With the right support and interventions, individuals can find relief from the burdens of their trauma, reclaiming their nights and enhancing their overall well-being.




